
Impact of Bacterial Keratitis on Output Care Hospital in Bangladesh
Mohammed Selim
Reza 1![]() , Md Rahimullah Miah 2
, Md Rahimullah Miah 2![]() , Md
Nazmul Islam 3
, Md
Nazmul Islam 3![]() , Jafrin
Sultana Silvy 4, Nizam Jamil
Hussain 1, Jorin Tasnim Parisha 4, Azima Aktar Jhuma 5
, Jafrin
Sultana Silvy 4, Nizam Jamil
Hussain 1, Jorin Tasnim Parisha 4, Azima Aktar Jhuma 5![]() , Md
Altaf Hossain 6
, Md
Altaf Hossain 6![]() , Md
Harunur Rashid 7
, Md
Harunur Rashid 7![]() , Shahriar
Hussain Chowdhury 8
, Shahriar
Hussain Chowdhury 8![]()
1 Department
of Ophthalmology, North East Medical College Hospital, Affiliated to Sylhet
Medical University, Sylhet, Bangladesh
2 Department
of Health Information Technology, North East Medical College Hospital,
affiliated to Sylhet Medical University, Sylhet, Bangladesh
3 Department of Nephrology, North East Medical College and Hospital, Affiliated to Sylhet Medical University, Sylhet, Bangladesh
4 Science Group, College Education Program, Sylhet Government Women’s College, Sylhet, National University, Gazipur, Bangladesh
5 Department of Microbiology, Sylhet MAG Osmani Medical College Hospital, Affiliated to Sylhet Medical University, Sylhet, Bangladesh
6 Department of Ophthalmology, Sylhet Women’s Medical College Hospital, Affiliated to Sylhet Medical University, Sylhet, Bangladesh
7 Department of Ophthalmology, Sylhet MAG Osmani Medical College Hospital, Affiliated to Sylhet Medical University, Sylhet, Bangladesh
8 Department of Dermatology & Venereology, North East Medical College and Hospital, Affiliated to Sylhet Medical University, Sylhet, Bangladesh
|
|
ABSTRACT |
||
|
Background Bacterial keratitis is a potentially fatal corneal infection worldwide. Its deleterious effects include sudden and rapid destruction of the cornea. The exact cause is still unknown to health authorities and ophthalmologists. Various studies have suggested different theories. Some studies have suggested that the spectrum of bacterial corneal pathogens is largely influenced by local microbial flora, geography, and climatic factors. Aims and Objectives The aim of this study is to determine the bacteriological patterns and predisposing factors of bacterial keratitis in outpatient settings. Methods A total of 45 male and female patients with bacterial keratitis were evaluated from January 2015 to December 2016 at the Department of Ophthalmology, MAG Osmani Medical College Hospital, Sylhet, a divisional city of Bangladesh. The study recorded the patients' socio-demographic information, pre-existing factors, and clinical presentation. Bacterial cultures were performed from corneal swabs in the laboratory. Results The age range of most patients was between 41 and 60 years (55.6%). The mean age of bacterial keratitis was 47.60 ± 17.14 (range, 18–71) years. The study showed that the male to female ratio was 1.25:1, which was close to 1. The study also showed that common predisposing factors were 62.2% trauma and 31.1% chronic dacryocystitis. The highest 57.8% Gram-positive bacteria predominated, and the lowest 42.2% Gram-negative bacteria. Out of the total isolates, 37.8% were Staphylococcus epidermidis, 26.7% Pseudomonas aeruginosa, 20.0% Staphylococcus aureus, 8.9% Escherichia coli, and 6.7% Klebsiella species. Conclusion The study concluded that trauma is the most important predisposing factor in bacterial keratitis. Gram-positive bacteria are the main isolates and common bacteria are Staphylococcus epidermidis, Pseudomonas aeruginosa and Staphylococcus aureus. This study suggests a new dynamic alternative approach to the upcoming eye care pathway to promote global eye protection related to advanced sensor technology and national health policies, which is aligned with the Sustainable Development Goals 2030. |
|||
|
Received 10 August 2025 Accepted 15 September 2025 Published 17 October 2025 Corresponding Author Mohammed
Selim Reza, drselimreza44@gmail.com DOI 10.29121/granthaalayah.v13.i9.2025.6340 Funding: This research
received no specific grant from any funding agency in the public, commercial,
or not-for-profit sectors. Copyright: © 2025 The
Author(s). This work is licensed under a Creative Commons
Attribution 4.0 International License. With the
license CC-BY, authors retain the copyright, allowing anyone to download,
reuse, re-print, modify, distribute, and/or copy their contribution. The work
must be properly attributed to its author.
|
|||
|
Keywords: Bacterial Keratitis, Predisposing
Factors, Clinical Profile, Bacteriological Profile |
|||
1. INTRODUCTION
The cornea is a very important organ that helps maintain eye health, sharp vision, attractive eyelashes, and a better quality of life Soleimani et al. (2023). It acts as a strong shield, protecting the eye from various unexpected infections and providing strong structural support while adapting to the harsh environment Bălășoiu et al. (2024). Bacterial keratitis is a sudden onset and chronic or transient infectious process of the cornea that presents as insidious progressive ulceration Al-Mujaini et al. (2009). It also has a variable tendency to appear as a rapidly deteriorating purulent infection of the corneal topography, anatomy or geographic areas Al-Mujaini et al. (2009). Microbial keratitis Estopinal and Ewald (2016),Truong et al. (2015) is an undesirable ophthalmic emergency that requires prompt and effective prevention, depending on the legal priority and existing circumstances, as it can progress rapidly, resulting in severe vision loss or corneal blindness Gurnani and Kaur (2025), Robaei and Watson (2014). Corneal scarring is also listed as the second leading cause of blindness and visual impairment Dandona et al. (2001), Dineen et al. (2007) in Asian countries, especially Bangladesh, India, Pakistan, and Sri Lanka, in the Watson Survey for Blindness and Visual Impairment, after cataracts Gurnani et al. (2021), Gurnani et al. (2021). In Bangladesh, 33.55% of cases of unilateral blindness have been reported as complications Cuesta et al. (2021) of corneal ulcers Khan and Haque (1985), Pakzad-Vaezi et al. (2015).
The ocular surface is commonly degraded by microbial invasion due to the multifaceted biochemical and physiological connections between the cornea, conjunctiva, lacrimal secretory apparatus, and precorneal tear film and the eyelids Bharathi et al. (2003). If the cornea's protective system is suddenly disrupted or the corneal epithelium ruptures, microbes are free to invade the cornea Benson and Lanier (1998). Microbial keratitis can be caused by viruses, bacteria, protozoa, fungi, and sensor technological, and the spectrum of microorganisms causing keratitis varies according to environmental location and climatic zone Bharathi et al. (2003). However, in most cases it is caused by bacteria, and bacterial keratitis accounts for 54% to 94.2% of all corneal infections Lichtinger et al. (2012). Bacterial keratitis is rare because it has no known predisposing cause. Until recently, most cases of bacterial keratitis were associated with eye trauma or ocular surface disease, including man-made technological sensor diseases Zemba et al. (2020). However, the sudden widespread use of contact lenses among younger generations Alipour et al. (2017) has led to a sharp increase in the incidence of contact lens-associated keratitis in specific GPS locations Christy et al. (2020). The spectrum of bacterial keratitis may also be predicted by geographic, climatic and wireless sensor tracking. There are substantial differences in keratitis profiles and technological secrets or digital conspiracies between populations living in rural, urban or remote areas, in developed countries, Western countries or developing countries Bourcier et al. (2003). Moreover, there is a lack of well-developed research. Bacterial culture from a fine corneal swab specimen is still the gold standard for the diagnosis of bacterial keratitis Soleimani et al. (2020), allowing the isolation of the causative bacteria [86]. However, due to various limitations, not all medical institutions are able to perform these tests. Therefore, empirical diagnosis is of great importance for physicians, researchers, and scientists to know the pathogenic microorganisms and the appropriate antibiotics to eradicate the infection Leck (2009) Hsiao et al. (2016). In the era of advanced satellite technology, little information is available on the frequency [106] of predisposing factors for bacterial keratitis and the demographic characteristics of those patients. The aim of the study was to identify predisposing factors Cruciani et al. (2009), to unravel the main symptom, and to define in a new way the clinical, sensorineural, and microbiological Bonnet et al. (2020) features Younger et al. (2012) of bacterial keratitis in our current practice.
2. Materials and Methods
This cross-sectional study was conducted from January 2015 to December 2016 at the Department of Ophthalmology, Sylhet MAG Osmani Medical College Hospital affiliated to Sylhet Medical University, Bangladesh. Forty-five patients with bacterial keratitis, aged 18 years and older and of both sexes, were included in this higher study. Patients with suspected viral keratitis (simple dendritic ulcers with loss of corneal sensation), vernal catarrhal shield corneal ulcers, neurotrophic corneal ulcers Reza et al. (2021), Reza et al. (2023), Reza et al. (2023), Chowdhury et al. (2023), Chu and Hu (2013) (painless ulcers without infiltration and minimal conjunctival congestion) Everts et al. (2011), Gurnani et al. (2020), and systemic diseases associated with keratitis were excluded from the study due to improved medical considerations, rapid recovery, expansion of advanced sensor technology, and environmental conditions Gurnani et al. (2022).
All patients were assessed by history, physical examination, and laboratory investigations during the study. Non-viral microbial keratitis Sand et al. (2015) was defined as damage to the corneal epithelium with underlying stromal infiltrates associated with signs of inflammation with or without hypopyon Hussain et al. (2012), Ung et al. (2019), Lievens et al. (2017). Visual acuity, corneal sensation, slit lamp examination, and direct ophthalmoscopy were performed to detect ocular disease.
The following information was obtained regarding risk factors, including age, gender, duration of symptoms at presentation, (duration and) corneal trauma (agricultural and non-agricultural), contact lens Lievens et al. (2017) wear, ocular surface disease (trichiasis, entropion, lagophthalmos, dry eye, blepharitis, etc.), topical steroid use, chronic dacryocystitis, diabetes mellitus, and vitamin A deficiency (vitamin A deficiency results in decreased epithelial integrity, xerosis, and active liquefaction necrosis of the corneal stroma).
Best-corrected visual acuity (BCVA) in Snellen format, ulcer size in mm along the highest dimension, and hypopyon (vertical height at 6 o'clock in mm) using a slit lamp were recorded at admission.
2.1. Bacterial Culture
Samples were collected from the base and edge of the ulcer using a sterile cotton swab soaked in sterile normal saline before application of local anesthetic by the ophthalmologist. Bacterial culture from corneal swabs Reza et al. (2021), Reza et al. (2023), Reza et al. (2023), Chowdhury et al. (2023), Giuliano et al. (2019) was performed in a convenient scientific manner at the Department of Microbiology, MAG Osmani Medical College, Sylhet.
The swab from the corneal wound was carefully and skillfully taken with a sterile cotton swab soaked in sterile normal saline and inoculated onto blood agar and MacConkey's agar media and incubated for 24 hours at 37°C. Bacteria grown on the culture media during observation were estimated by colony characteristics against each organism.
Isolates were further identified using standard identification protocols such as Gram's staining, motility test and biochemical tests Collee et al. (1996), Reza et al. (2021), Reza et al. (2023), Reza et al. (2023), Chowdhury et al. (2023). Catalase test, coagulase test and mannitol fermentation test were performed to identify S. aureus and S. epidermidis. Members of the Enterobacteriaceae such as E. coli, Klebsiella and Pseudomonas were identified by their sugar fermentation, indole production and citrate utilization characteristics. All patients were treated conservatively with oral ciprofloxacin, moxifloxacin eye drops and atropine eye drops to increase mental and physical courage in the patients.
2.2. Statistical Analysis
Data were manually processed and analyzed using MS Office Suite, SPSS (Statistical Package for Social Sciences) version 31.0. Quantitative data were expressed by means and standard deviation. Qualitative data were expressed by frequencies and percentages. All aggregated data were prepared for presentation and interpretation.
2.3. Ethical Consideration
Informed written consent was obtained after detailed discussion of the objectives of the study from the health administration. Before the study began, approval of the research protocol was obtained from the ethics committee of MAG Osmani Medical College Hospital, Sylhet, Bangladesh, and the research guidelines of that committee were followed.
3. Results
The study found that the maximum number of patients with bacterial keratitis was 10, aged 41-50 years, and the minimum number was 2, aged 11-20 years, which as shown in Figure 1.
Figure 1
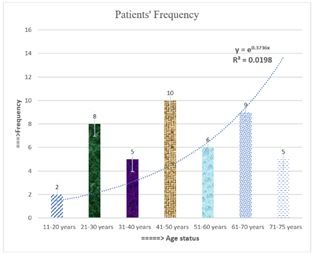
|
Figure 1 Patients’ age Status with Bacterial Keratitis in the Study Area |
The age of the patients with bacterial keratitis ranged from 18 years to 71 years with the mean age of 47.60 ± 17.14 years with equal male and female (1.25:1). Majority of patients were between 41 and 60 years (55.6%) Table 1. Common predisposing factors of bacterial keratitis were trauma (62.2%) and chronic dacryocystitis (31.1%) Table 2. Clinical features were watering and redness of eye (100.0%), photophobia (95.6%), pain or burning sensation (70.5%) and dimness of vision (71.1%); and the signs were cilliary congestion (100.0%), corneal opacity (100.0%), lid swelling (93.3%), blepharspasm (93.3%) and corneal vascularization (91.1%) Table 3.
Table 1
|
Table 1 Socio-Demographic Characteristics of the Patients with Bacterial Keratitis (n=45) |
||
|
Variables |
Percentage |
|
|
Age |
||
|
11-20 years |
4.4 |
|
|
21-30 years |
17.8 |
|
|
31-40 years |
11.1 |
|
|
41-50 years |
22.2 |
|
|
51-60 years |
13.3 |
|
|
61-70 years |
20 |
|
|
71-75 years |
11.1 |
|
|
Sex |
||
|
Male |
55.6 |
|
|
Female |
20 |
44.4 |
Table 2
|
Table 2 Showing Distribution of Patients According to Predisposing Factors with Fungal |
||
|
keratitis (n=45) |
||
|
Predisposing Factors |
Frequency |
Percentage |
|
Trauma |
28 |
62.2 |
|
Paddy |
20 |
44.4 |
|
Leaf |
5 |
11.1 |
|
Soil |
2 |
4.4 |
|
Blunt trauma |
1 |
2.2 |
|
Chronic dacryocystitis |
14 |
31.1 |
|
Entropion |
2 |
4.4 |
|
Exposure keratitis |
1 |
2.2 |
|
Total |
45 |
100 |
Table 3
|
Table 3 Showing Distribution of patients According to Clinical Presentation of Bacterial Keratitis (n=45) |
||
|
Clinical Presentation |
Frequency |
Percentage |
|
Symptoms |
||
|
Watering and Redness |
45 |
100 |
|
Pain or burning
sensation |
31 |
70.5 |
|
Dimness of vision |
32 |
71.1 |
|
Photophobia |
43 |
95.6 |
|
Signs |
||
|
Blepharspasm |
42 |
93.3 |
|
Lid swelling |
42 |
93.3 |
|
Cilliary congestion |
45 |
100 |
|
Corneal opacity |
45 |
100 |
|
Corneal
vascularization |
44 |
97.8 |
|
Hypopyon |
5 |
11.1 |
Gram-positive organisms (n=26, 57.8%) of which Staphylococcus epidermidis in 17 (38%), Staphylococcus aureus in 9 (20%); while gram negative organisms (n=19, 42.2%) of which Pseudomonas aeruginosa in 12 (27%), Escherichia coli in 4 (9%) and Klebsiella species in 3 (6.7%) cases, which as shown in Figure 2.
Figure 2
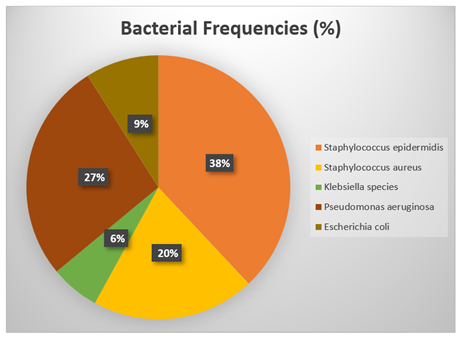
|
Figure 2 Showing Isolated Bacteria in Patients with Bacterial Keratitis |
Bacterial keratitis occurs in any age with nearly equal sex distribution. Trauma is the most important predisposing factor in bacterial keratitis. Gram-positive organism are predominant isolates and common isolates are Staphylococcus epidermidis, Pseudomonas aeruginosa and Staphylococcus aureus. Avoidance of ocular trauma may prevent bacterial keratitis. However further large-scale multi-centre study is warranted.
4. Discussion
The study shows that infectious keratitis Austin et al. (2017), Solanki et al. (2015) is a common sight-threatening eye emergency Acharya et al. (2019), Vemuganti et al. (2011). Studies have shown that bacterial keratitis is an ocular emergency, causing pain, photophobia, and redness. If left untreated, in addition to scarring, it can lead to endophthalmitis and even corneal perforation and blindness Shoja and Manaviat (2004), Li et al. (2024).
The safe use of advanced sensor technologies in appropriate environments depends on the accurate and rapid identification of the causative organism Ray et al. (2013). The epidemiology of the causative agent in microbial keratitis varies significantly from individual to individual, from country to country, and even from region to region within the same community or country Kumar, A., Pandya, S., Kavathia et al. (2011), Young et al. (2013). Recent studies have shown that people or animals with active photoreceptors are infected with bacterial/microbial keratitis by tracking them with GPS sensors in connected cloud sensor networks Miah et al. (2022a).
4.1. Equal Distribution
In this study, the age of patients with bacterial keratitis ranged from 18 to 71 years, with a mean age of 47.60 ± 17.14 years. Kaliamurthy et al. Kaliamurthy et al. (2013) found that the mean age of patients with bacterial keratitis was 45.7 ± 16.6 years. Boursier et al. Bourcier et al. (2003) found that the age of patients ranged from 6 months to 94 years (mean age 39 years). This study found that there was an almost equal distribution of males and females in bacterial keratitis (1.25:1). In the study by Boursier et al., the gender distribution of bacterial keratitis was close to 1:1 (152 males and 139 females) Bourcier et al. (2003), while Kaliamurthy et al. Kaliamurthy et al. (2013) found that 58.7% of patients with bacterial keratitis were male and 41.3% female. Higher studies have shown that GPS sensor tracking infects all types of eye diseases, including bacterial keratitis, in men, women, and children of all ages.
4.2. Predisposing Factors
Common predisposing factors for bacterial keratitis were trauma (62.2%) and chronic dacryocystitis (31.1%). In the 1980s, ocular trauma was the most common predisposing factor in young patients Musch et al. (1983). However, studies have shown that corneal ulceration Mah-Sadorra et al. (2005) following trauma is a much more common predisposing factor in rural areas or low-income countries, where it accounts for up to 77.5% of cases Vajpayee et al. (2000). Other studies have shown that contact lens wear was the most common predisposing factor, followed by ocular surface disorders and ocular trauma Bourcier et al. (2003).
4.3. Invasive Potential
According to the results of advanced research, the ability of an organism to adhere to the edge or base of an epithelial defect, to grow and to be interested in its pathogenicity, is a sign of its ability to invade the stroma despite adequate host defenses; previous researchers or scientists have noted that S. aureus, S. pneumoniae and P. aeruginosa are examples of bacteria with this invasive potential Kaliamurthy et al. (2013).
In this study, Gram-positive bacteria predominated (57.8%) while Gram-negative bacteria were 42.2%, which is consistent with the present and previous studies. Gram-positive bacteria were Staphylococcus epidermidis (37.8%) and Staphylococcus aureus (20.0%); whereas Gram-negative bacteria were Pseudomonas aeruginosa (26.7%), Escherichia coli (8.9%) and Klebsiella species (6.7%), which validates the study.
Previous researchers Ahmed et al. Ahmed et al. (2010) found that the main bacterial isolates were Staphylococcus epidermidis (32.85%) followed by Staphylococcus aureus (26.15%) and Pseudomonas spp. (20%). A review of the developed research literature found that most studies from developed countries listed Staphylococcus epidermidis as the main cause of bacterial keratitis Schaefer et al. (2001), but no significant studies on advanced sensor technology were highlighted, while the misuse of GPS sensor technology was unexpected.
It is also noteworthy that Kaliamurthy et al. Kaliamurthy et al. (2013) found that 82% of the isolates in the culture were Gram-positive bacteria and 18% were Gram-negative bacteria. The most common bacterial pathogen was various species of Staphylococcus, which accounted for 64.5% of all positive bacterial cultures, followed by Streptococcus spp. (12.3%), Pseudomonas aeruginosa (9.7%), Bacillus spp. (5.2%), Acinetobacter spp. (4.6%), and Aeromonas spp. (1.49%). Enterobacter spp., Klebsiella pneumoniae, Serratia marcescens, and Flavobacterium spp. were the least frequently isolated organisms in their series.
Other studies have shown that Staphylococcus epidermidis and Staphylococcus aureus form a combination of the outer surface of the eye, as these bacteria can invade the corneal tissue due to antimicrobial and/or corticosteroid therapy or trauma. Currently, endemic bacteria such as coagulase-negative staphylococcus are increasingly isolated in bacterial keratitis and have become the bacterial pathogens responsible for most infectious keratitis Bourcier et al. (2003), Austin et al. (2017). However, mixed studies have shown that viral keratitis, followed by bacterial keratitis, was the most frequent cause of microbial keratitis Young et al. (2013), Jin et al. (2017), Sakr et al. (2023).
4.4. Innovative Treatment Approach
Early diagnosis and intensive treatment are essential for the management of bacterial keratitis Mishra and Meyer (2022) in a scientific manner and with the help of advanced medical technology, so that the patient can recover as soon as possible Mishra and Meyer (2022). Bacterial keratitis is a serious eye infection that can cause stern vision loss if not treated early Bouhenni et al. (2015). An innovative treatment can apply to recover bacterial keratitis Wong et al. (2012). There are also another therapeutic methos illustrated Nguyen et al. (2021), Wen et al. (2022). Clinical improvement was observed immediately after treatment with the necessary antibiotic drops, tapering, transplant and BKRAST Zhai et al. (2021). Bacterial keratitis treats with BKRAST model according to treatment algorithms, which as shown in Figure 3. The BKRAST implies Bacterial keratitis Recovery through Advanced Sensor Technology and ISNAPHO (Impact of Sensor Networks on Animals, Plants, Humans and Objects) is an experiment through sensor tracking on humans, animals, plants and others.
Figure 3

|
Figure 3 ISNAPHO Effect along with Recovery BKRAST Model Miah et al. (2022a) |
4.5. Advanced Ophthalmic Research
Modern research has shown that astronauts suffer from SANS (Spaceflight Associated Neuro-Ocular Syndrome) due to unwanted causes Yang et al. (2022). Different studies have suggested that SANS is a disease similar to sensor keratitis Miah et al. (2021a), which is a scientific finding Miah et al. (2022a), because, using GPS sensor tracking, all types of eye diseases are caused in humans or animals if photoreceptors are active at a specific location Miah et al. (2021a). Corneal protection is extremely important to prevent sudden abrasion and possible complications due to GPS sensor technical tracking Grixti et al. (2013).
Moreover, space experts, policymakers and health professionals have been unable to determine the root cause of astronauts' illnesses for several years. This research confirms that all types of eye diseases are caused by man-made sensor technology, which is spread through GPS sensor tracking. Health technologists have attributed the disease to sensor technology tracking Miah et al. (2023), which has been attributed to digital pathogens, which are transmitted to a person's eyes via photoreceptors due to GPS sensor tracking Miah et al. (2022). Physiological challenges in space include microgravity, radiation, environmental stress, and the misuse of GPS satellite sensor technology, which unexpectedly increase the risk of ocular surface disease in astronauts Lee et al. (2025).
4.6. Risks
Waiting in a certain place for a long time or walking on the street due to GPS sensor tracking by cybercriminals can cause bacterial keratitis and other sensor diseases in humans or animals, which increases the risk of serious sensor diseases in their eyes Miah et al. (2021a). In addition, prolonged contact lens wear Lievens et al. (2017), Alipour et al. (2017), poor hygiene Stellwagen et al. (2020), sudden corneal injury, severe eye pain Miah et al. (2022a) in people who have had previous eye surgery, worsening of ocular surface diseases, abnormal eyelids and sudden extreme redness, sudden decrease in the body's immune system, elderly people who are more susceptible due to systemic immunosuppression, and prolonged use of corticosteroid eye drops are also at risk Miah et al. (in press). Bacterial keratitis as well as technological environmental diseases can affect women, men and children in certain GPS locations Reza et al. (2021),Chowdhury and Miah (2024). To avoid this risk, the research makes everyone aware to protect themselves from environmental diseases. Bacterial keratitis is very painful for men, women, and children, usually associated with serious risk factors that disrupt the epithelial integrity of the cornea Gurnani and Kaur (2025).
4.7. Policy Implication
National and international health policies Miah et al. (2022a), Miah et al. (2022i), advanced sensor technology policies, environmental health policies Miah et al. (2021), Miah et al. (2022c), climate policies Miah et al.(2023f), Miah et al. (2021h), food and nutrition policies Miah (2013), drug policies Miah et al, (2023) and political commitment Miah et al. (2023k),Miah et al. (2023) are closely related to improved treatment methods for bacterial keratitis and various other diseases. But no country in the world has yet implemented an effective integrated and meaningful modern health policy Miah et al. (2022), Miah et al. (2023n).
All types of keratitis, including bacterial keratitis, require a unique health policy that will include alternative treatment options, unique research, and advanced nutritional support innovations. Due to the misuse of GPS satellite sensors, people and animals around the world are facing serious digital health risks, including eye diseases. The threat of sensor diseases in the eyes of the people by health criminals in almost every country due to the misuse of cloud sensor networks in the world, the sudden digital bullet hit on the eyes of healthy people at a specific GPS location, the widespread spread of eye diseases under the influence of man-made artificial climate crises, sudden fatal eye diseases in technological earthquakes and unexpected costs in eye treatment of the people due to floods, health care in remote settlements, the terrible pandemics of environmental diseases in wireless sensor tracking, the isolation of advanced health communication with neighboring countries, and the sharp decline of national, regional, and global health economies - all these are digital health criminal activities.
Therefore, governments, ophthalmologists, sensor technologists, and policymakers need to develop sustainable ways to quickly remedy man-made sensor eye diseases and take effective legal and policy measures to prosecute health criminals Miah et al. (2022). To raise public awareness about man-made eye diseases in the media about the use and misuse of satellite sensor technology in daily life so that the administration can take quick and effective action against health criminals. Furthermore, in line with the impact of contemporary sensor technology and health policies, formulating and implementing integrated public health policies to ensure the use of safe sensor technology in the eradication of man-made eye diseases, especially bacterial keratitis, can yield acceptable results at all recovery levels. The study also noted that the use of safe sensor technology, observance of religious activities of individuals, speedy trial of health criminals, digital health support systems, coordination with various departments, and cooperation with national and international organizations are essential to achieve the national health policy and the Sustainable Development Goals 2030 Miah et al. (in press).
4.8. Deterrence and Patient Education
Bacterial keratitis is a rare, serious, environmental, congenital Gurnani et al. (2020) and sensitive eye disease that causes inflammation of the cornea Willcox (2007) due to bacterial infection or GPS sensor tracking in the eye Miah et al. (2022a), Miah et al. (2022i). With other eye diseases, the patient may develop complications such as vision loss. To prevent this complication, research has shown that taking the following Top-ten measures can prevent eye and related diseases, resulting in faster recovery of the patient, such as:
1) Do not sleep with a mobile phone near or in an active sensor network connection when GPS location is active Miah et al. (2021a),
2) Do not sleep with contact lenses in the eyes in both light and dark environments with wireless sensor networks Miah et al. (2021a),Miah et al. (2022a),
3) Do not talk after sleeping in bed or in a specific place, otherwise, cybercriminals can spread the sensor disease more intensely in the affected person's body by detecting the GPS location in combination with the patient's photoreceptors and magnetoreceptors Miah et al. (2021a), Miah et al. (2022i), Cope et al. (2018).
4) Do not use additional contact lenses in a specific GPS location without consulting an ophthalmologist or doctor, a health sensor specialist Miah et al. (2021a), Miah et al. (2022a) and nutritionist.
5) If individuals suddenly feel pain or discomfort in their eyes at a specific GPS location, move quickly and wear sunglasses and stay in the sensor network isolator zone Miah et al. (2021a),
6) Before putting lenses in your eyes, wash your hands and face thoroughly and drink some water to calm yourself down Reza et al. (2021), Reza et al. (2023), Reza et al. (2023a), Chowdhury et al. (2023),
7) Wear sunglasses in the bathroom or in specific places as needed, which can be used daily to get rid of eye diseases Miah et al. (2021a), Miah et al. (2022a),
8) Do not use tap water as a lens solution, which can worsen your vision problems. Read religious books or enjoyable books at special times, which will increase the protein sensors of the eyes and vision Miah et al. (2022a),
9) If you suddenly feel pain, blurring or itching in your eyes, it is very good to solve it in alternative ways without your own hands, because due to retinal Gurnani et al. (2021) scanning and fingerprinting, cybercriminals can misuse the victim's e-body code by touching their hands on the eyes to cause various sensor diseases in the eyes and other organs Miah et al. (2022a),
10) Follow the EDRAST (Eye Disease Recovery through Advanced Sensor Technology) model, wear anti-radiation sunglasses on the eyes, set up a body position sensor network isolator and use a "Personal Body Sensor Area Network Control Unit" ((PANCU) or anti-sensor device on the body Miah et al. (2021a), Miah et al. (2022a), which can prevent bacterial keratitis.
In addition to bacterial keratitis, various sensor diseases such as diabetes mellitus Miah et al.(2020a), Miah et al. (2021b), thyroid disease, respiratory disorders Miah et al. (2022g) (ARDS implies acute respiratory distress syndrome) problem syndrome), vitamin A deficiency, acute pain Miah et al. (2021a), rheumatoid arthritis Miah et al. (2021a), glaucoma Chowdhury et al. (2023), Sjogren's syndrome Miah et al. (2022g), headaches, sensor retinoblastoma Miah et al. (2021a), Miah et al. (2023n), COVID-19 Miah et al. (2021), Miah (2024), Miah et al. (2022), Miah et al. (2022a), Miah et al. (2022h), Miah et al. (2021g), Miah et al. (2021d), Miah et al. (2021e), Miah et al. (2020), Chowdhury and Miah (2024), dermal and environmental diseases [28; Miah et al. (2023), Miah et al. (2023e) and Stevens-Johnson syndrome Miah et al. (2021a) spread through GPS sensor tracking or scattering.
4.9. Limitations
Limitations of the study were (1) This study was conducted in single hospital, (2) Sampling was non-random, (3) Sample size was small, (4) No network isolator at patient zone, and (5) Limit of personal body area sensor network control unit.
4.10. Recommendations
The following recommendations should be followed by the general public, patients and higher authorities.
1) The individual should follow DRAST guidelines when receiving sudden signals from GPS sensor tracking or scattering on his/her eyes.
2) If any problematic symptoms occur, he/she should carefully avoid eye injuries and immediately consult an eye specialist or ophthalmologist.
3) He lives in a life-managed health environment, in a happy, joyful and user-friendly sensor network.
4) Higher authorities should change national and global health policies in accordance with the expansion of advanced sensor technology and research findings.
The Government of each State should restrict the individual’s retina scanning and fingerprint coding during passport and NID card receiving.
5. Conclusion
Bacterial keratitis is a highly sensitive and risky condition for eyes of any age, with people of almost equal genders, which is controlled by health criminals from a specific location through wireless sensor technology. Therefore, unique care and advanced treatment are required for the patient by overcoming technological and environmental challenges. However, conventional treatment is not standardized and affordable, and ophthalmologists may lack the skills and unique research to cure the patient quickly. Therefore, it is essential to develop new drugs, technological support, advanced research and delivery methods that are more suitable for treating eye disease conditions and preserving the corneal epithelium. Finally, it is necessary to develop a novel non-drug approach and alternative way to treat keratitis, so that it can overcome the conventional challenges and achieve a faster recovery.
6. Declarations
Author Contributions
Main author designed the study, collected the data and drafted the article, and co-authors designed the study and revised the article critically. All the authors finally contributed to the final approval of the version to be published.
Data Availability
The data being used to support the findings of this research work are available from the corresponding author upon request.
Ethical Consideration
The Ethical Consideration of this study with reference was obtained after detailed discussion of the objectives of the study from the health administration. Before the study began, approval of the research protocol was obtained from the ethics committee of MAG Osmani Medical College Hospital, affiliated to Sylhet Medical University, Sylhet, Bangladesh.
CONFLICT OF INTERESTS
None.
ACKNOWLEDGMENTS
We are grateful to the patients who gave their consent for taking part of this study. The authors also thank to Director, Sylhet MAG Osmani Medical College, Sylhet for giving permission to collect data. The authors acknowledged the authority of Sylhet Medical University and Shahjalal University of Science and Technology, Sylhet, Bangladesh for the completion of MD degree. The authors are also grateful to the authority of the Ministry of Health and Family Welfare, Government of People’s Republic of Bangladesh, for kind support on research work. The authors acknowledged the authority of North East Medical College & Hospital (NEMCH), affiliated to Sylhet Medical University, Sylhet, Bangladesh for kind support.
REFERENCES
Acharya, M., Farooqui, J. H., Jain, S., & Mathur, U. (2019). Pearls and Paradigms in Infective Keratitis. Romanian Journal of Ophthalmology, 63(2), 119–127. https://doi.org/10.22336/rjo.2019.18
Ahmed, S., Ghosh, A., Hassan, S. A., Tarafder, S., & Miah, M. R. A. (2010). Predisposing Factors and Aetiologic Diagnosis of Infectious Corneal Ulcer. Bangladesh Journal of Medical Microbiology, 4(1), 28–31. https://doi.org/10.3329/bjmm.v4i1.8466
Alipour, F., Khaheshi, S., Soleimanzadeh, M., Heidarzadeh, S., & Heydarzadeh, S. (2017). Contact Lens-Related Complications : A Review. Journal of Ophthalmic & Vision Research, 12(2), 193–204.
Al-Mujaini, A., Al-Kharusi, N., Thakral, A., & Wali, U. K. (2009). Bacterial Keratitis: Perspective on Epidemiology, Clinico-Pathogenesis, Diagnosis and Treatment. Sultan Qaboos University Medical Journal, 9(2), 184–195. https://doi.org/10.18295/2075-0528.2789
Austin, A., Lietman, T., & Rose-Nussbaumer, J. (2017). Update on the Management of Infectious Keratitis. Ophthalmology, 124(11), 1678–1689. https://doi.org/10.1016/j.ophtha.2017.05.012
Austin, A., Lietman, T., & Rose-Nussbaumer, J. (2017). Update on The Management of Infectious Keratitis. Ophthalmology, 124(11), 1678–1689. https://doi.org/10.1016/j.ophtha.2017.05.012
Bălășoiu, A. T., Bălășoiu, M., Zlatian, O. M., & Ghenea, A. E. (2024). Bacterial and Fungal Keratitis in a Tertiary Care Hospital from Romania. Microorganisms, 12(4), 787. https://doi.org/10.3390/microorganisms12040787
Benson, W. H., & Lanier, J. D. (1998). Current Diagnosis and Treatment of Corneal Ulcers. Current Opinion in Ophthalmology, 9(4), 45–49. https://doi.org/10.1097/00055735-199808000-00008
Bharathi, M. J., Ramakrishnan, R., Vasu, S., Meenakshi, R., & Palaniappan, R. (2003). Epidemiological Characteristics and Laboratory Diagnosis of Fungal Keratitis: A Three-Year Study. Indian Journal of Ophthalmology, 51, 315–321.
Bonnet, M., Lagier, J. C., Raoult, D., & Khelaifia, S. (2020). Bacterial Culture Through Selective and Non-Selective Conditions : The Evolution Of Culture Media in Clinical Microbiology. New Microbes and New Infections, 34, 100622. https://doi.org/10.1016/j.nmni.2019.100622
Bouhenni, R., Dunmire, J., Rowe, T., & Bates, J. (2015). Proteomics in the Study of Bacterial Keratitis. Proteomes, 3(4), 496–511. https://doi.org/10.3390/proteomes3040496
Bourcier, T., Thomas, F., Borderie, V., Chaumeil, C., & Laroche, L. (2003). Bacterial Keratitis: Predisposing Factors, Clinical and Microbiological Review of 300 Cases. British Journal of Ophthalmology, 87(7), 834–838. https://doi.org/10.1136/bjo.87.7.834
Chowdhury, M. A. K., Reza, M. S., Miah, M. R., Jahangir, S. M., Chowdhury, M. T. T., & Ahmed, J. U. (2023). Effects of Pharmacological Agents on Glaucoma in Daily Life. International Journal of Optics and Applications, 9(1), 1–21. https://doi.org/10.5923/j.optics.20230901.01
Chowdhury, S. H., Miah, M. R., et al. (2024). Performance Services for COVID-19 with Private Medical College Hospitals. Global Journal of Health Science, 16(1), 46. https://doi.org/10.5539/gjhs.v16n1p46
Christy, J., Gurnani, B., Kaur, K., & Moutappa, F. (2020). Contact Lens Warpage: Lost but Found. Indian Journal of Ophthalmology, 68(8), 1662. https://doi.org/10.4103/ijo.IJO_2034_19
Chu, H. S., & Hu, F. R. (2013). Non-Tuberculous Mycobacterial Keratitis. Clinical Microbiology and Infection, 19(3), 221–226. https://doi.org/10.1111/1469-0691.12094
Collee, J. G., Duguid, J. P., Fraser, A. G., Marmion, B. P., & Simmons, A. (1996). Laboratory Strategies in the Diagnosis of Infective Syndromes. In J. G. Collee, A. G. Fraser, B. P. Marmion, & A. Simmons (Eds.), Mackie & McCartney practical medical microbiology (14th ed., pp. 53–93). Churchill Livingstone.
Cope, J. R., Konne, N. M., Jacobs, D. S., Dhaliwal, D. K., Rhee, M. K., Yin, J., & Steinemann, T. L. (2018). Corneal Infections Associated with Sleeping in Contact Lenses—Six Cases, United States, 2016–2018. MMWR. Morbidity and Mortality Weekly Report, 67(32), 877–881. https://doi.org/10.15585/mmwr.mm6732a2
Cruciani, F., Cuozzo, G., Di Pillo, S., & Cavallaro, M. (2009). Predisposing Factors, Clinical and Microbiological Aspects of Bacterial Keratitis: A Clinical Study. Clinica Terapeutica, 160(3), 207–210.
Cuesta Chasco, G., Carreras-Castañer, X., Zboromyrska, Y., Pitart, C., Palma-Carvajal, F., Bosch, J., & Figueroa-Vercellino, J. P. (2021). Adult Gonococcal Conjunctivitis: Prevalence, Clinical Features and Complications. Journal of Medical Microbiology, 70(9), 001416. https://doi.org/10.1099/jmm.0.001416
Dandona, L., Dandona, R., Srinivas, M., Giridhar, P., Vilas, K., Prasad, M. N., et al. (2001). Blindness in the Indian State of Andhra Pradesh. Investigative Ophthalmology & Visual Science, 42, 908–916.
Dineen, B. P., Bourne, R. R. A., Ali, S. M., Huq, D. M. N., & Johnson, G. J. (2003). Prevalence and Causes of Blindness and Visual Impairment in Bangladeshi Adults—Results of the National Blindness and Low Vision Survey of Bangladesh. British Journal of Ophthalmology, 87(7), 820–828. https://doi.org/10.1136/bjo.87.7.820
Dineen, B., Bourne, R. R., Jadoon, Z., Shah, S. P., Khan, M. A., Foster, A., et al. (2007). Causes of Blindness and Visual Impairment in Pakistan : The Pakistan National Blindness and Visual Impairment Survey. British Journal of Ophthalmology, 91(8), 1005–1010. https://doi.org/10.1136/bjo.2006.108035
Estopinal, C. B., & Ewald, M. D. (2016). Geographic Disparities in the Etiology of Bacterial and Fungal Keratitis in the United States of America. Seminars in Ophthalmology, 31(4), 345–352. https://doi.org/10.3109/08820538.2016.1154173
Everts, R. J., Barnett, T., &
Lahood, B. R. (2011). The Utility of Routine
Conjunctival Swabs in Management of Conjunctivitis. The New Zealand Medical
Journal, 124(1328), 64–71.
Giuliano, C., Patel, C. R., & Kale-Pradhan, P. B. (2019). A Guide to Bacterial Culture Identification and Results Interpretation. P & T, 44(4), 192–200.
Grixti, A., Sadri, M., & Watts, M. T. (2013). Corneal Protection During General Anesthesia For Nonocular Surgery. The Ocular Surface, 11(2), 109–118. https://doi.org/10.1016/j.jtos.2012.10.003
Gurnani, B., & Kaur, K. (2020). Rare Traumatic Anterior Dislocation of Capsular Tension Ring–Intraocular Lens Complex In-Toto. Indian Journal of Ophthalmology, 68(11), 2529. https://doi.org/10.4103/ijo.IJO_807_20
Gurnani, B., & Kaur, K. (2025). Bacterial Keratitis. In Statpearls. StatPearls Publishing.
Gurnani, B., & Kaur, K. (2025). Bacterial Keratitis. In StatPearls. StatPearls Publishing. (Original work published 2023)
Gurnani, B., Kaur, K., & Gireesh, P. (2020). Rare Coexistence of Bilateral Congenital Sutural and Cortical Blue Dot Cataracts. Journal of Pediatric Ophthalmology & Strabismus, 57(1), 68. https://doi.org/10.3928/01913913-20191011-01
Gurnani, B., Kaur, K., & Gireesh, P. (2021). A Rare Presentation of Anterior Dislocation of Calcified Capsular Bag in a Spontaneously Absorbed Cataractous Eye. Oman Journal of Ophthalmology, 14(2), 120–121. https://doi.org/10.4103/ojo.OJO_65_2019
Gurnani, B., Kaur, K., & Sekaran, S. (2021). First Case of Coloboma, Lens Neovascularization, Traumatic Cataract, and Retinal Detachment in a Young Asian Female. Clinical Case Reports, 9(9), e04743. https://doi.org/10.1002/ccr3.4743
Gurnani, B., Narayana, S., Christy, J., Rajkumar, P., Kaur, K., & Gubert, J. (2022). Successful Management of Pediatric Pythium Insidiosum Keratitis with Cyanoacrylate Glue, Linezolid, and Azithromycin: Rare Case Report. European Journal of Ophthalmology, 32(5), NP87–NP91. https://doi.org/10.1177/11206721211006564
Hsiao, C.-H., Sun, C.-C., Yeh, L.-K., Ma, D. H., Chen, P.-Y., Lin, H.-C., et al. (2016). Shifting Trends in Bacterial Keratitis in Taiwan : A 10-year Review in a Tertiary-Care Hospital. Cornea, 35(3), 313–317. https://doi.org/10.1097/ICO.0000000000000734
Hussain, I., Khan, B. S., Soni, M., Iqbal, M., & Habibullah. (2012). Non-viral microbial keratitis: Etiology, Clinical Features and Visual Outcome. Journal of the College of Physicians and Surgeons Pakistan, 22(3), 151–154.
Jin, H., Parker, W. T., Law, N. W., Clarke, C. L., Gisseman, J. D., Pflugfelder, S. C., Wang, L., & Al-Mohtaseb, Z. N. (2017). Evolving Risk Factors and Antibiotic Sensitivity Patterns for Microbial Keratitis at a Large County Hospital. British Journal of Ophthalmology, 101(11), 1483–1487. https://doi.org/10.1136/bjophthalmol-2016-310026
Kaliamurthy, J., Kalavathy, C. M., Parmar, P., Nelson, J. C. A., & Thomas, P. A. (2013). Spectrum of Bacterial Keratitis at a Tertiary Eye Care Centre in India. BioMed Research International, 2013, Article 181564. https://doi.org/10.1155/2013/181564
Khan, M. U., & Haque, M. R.
(1985). Prevalence and Causes of Blindness in Rural
Bangladesh. Indian Journal of Medical Research, 82, 257–262.
Kumar, A., Pandya, S., Kavathia,
G., Antala, S., Madan, M., & Javdekar, T. (2011). Microbial Keratitis in Gujarat, Western India: Findings from 200
cases. Pan African Medical Journal, 10, 48.
Leck, A. (2009). Taking a Corneal Scrape and Making a Diagnosis. Community Eye Health, 22(71), 42–43.
Lee, R., Kumar, R., Shah, J., Ong, J., Waisberg, E., & Tavakkoli, A. (2025). Tear Film and Keratitis in Space: Fluid Dynamics and Nanomedicine Strategies for Ocular Protection in Microgravity. Pharmaceutics, 17(7), 847. https://doi.org/10.3390/pharmaceutics17070847
Li, Z., Xie, H., Wang, Z., Li, D., Chen, K., Zong, X., Qiang, W., Wen, F., Deng, Z., Chen, L., Li, H., Dong, H., Wu, P., Sun, T., Cheng, Y., Yang, Y., Xue, J., Zheng, Q., Jiang, J., & Chen, W. (2024). Deep Learning For Multi-Type Infectious Keratitis Diagnosis: A Nationwide, Cross-Sectional, Multicenter Study. NPJ Digital Medicine, 7, 181. https://doi.org/10.1038/s41746-024-01174-w
Lichtinger, A., Yeung, S. N., Kim, P., Iovieno, A., Elbaz, U., Ku, J. Y., et al. (2012). Shifting Trends in Bacterial Keratitis in Toronto : An 11-Year Review. Ophthalmology, 119(9), 1785–1790. https://doi.org/10.1016/j.ophtha.2012.03.031
Lievens, C. W., Cilimberg, K. C., & Moore, A. (2017). Contact Lens Care Tips for Patients : An Optometrist’s Perspective. Clinical Optometry, 9, 113–121. https://doi.org/10.2147/OPTO.S139651
Mah-Sadorra, J. H., Najjar, D. M., Rapuano, C. J., Laibson, P. R., & Cohen, E. J. (2005). Serratia Corneal Ulcers: A Retrospective Clinical Study. Cornea, 24, 793–800. https://doi.org/10.1097/01.ico.0000159738.06167.88
Miah, M. R. (2013). Enhancing Food Security Through Acclimatized Species Domestication in the Haor Region. ABC Journal of Advanced Research, 2(1), 49–65. https://doi.org/10.18034/abcjar.v2i1.19
Miah, M. R. (2024). Discovery of coronavirus (Book). Scientific & Academic Publishing.
Miah, M. R., Alam, M. S., Hasan, M. M., Parisha, J. T., Sayok, A. K., Rahman, M. S., Sharif, M. A., & Uddin, M. B. (2022c). Scientific Environmental Governance to Accelerate Sustainable Biodiversity Management. Advances in Life Sciences, 11(1), 1–16. https://doi.org/10.5923/j.als.20221101.01
Miah, M. R., Chowdhury, S. H., Parisha, J. T., Rashid, M. M., Hassan, M. M., & Sayok, A. K. (2023e). Impact of Radiofrequency Tracking on Body Surfaces for Acute Exacerbations of Skin Disease. American Journal of Dermatology and Venereology, 12(1), 1–9. https://doi.org/10.5923/j.ajdv.20231201.01
Miah, M. R., Hannan, M. A., Rahman, A. A. M. S., Khan, M. S., Hossain, M. M., Rahman, I. T., Hossain, M. S., Shahriar, C. S., Uddin, M. B., Talukdar, M. T. H., Alam, M. S., Hossain, S. A. M. I., Samdany, A. A., Chowdhury, S. H., & Sayok, A. K. (2021b). Processed Radio Frequency Towards Pancreas Enhancing the Deadly Diabetes Worldwide. Journal of Endocrinology Research, 3(1), 1–20. https://doi.org/10.30564/jer.v3i1.2826
Miah, M. R., Hasan, M. M., Hannan, M. A., Parisa, J. T., Uddin, M. J., Uddin, M. B., Rahman, A. A. M. S., Hossain, S. A. M. I., Sharif, M. A., Akhtar, F., Shamsuddin, M. A. S., Alam, M. S. E., Alam, M. S., Abdullah, F., Rahman, M. S., Uddin, M. B., Shahriar, C. S., Sayok, A. K., Begum, M., … Chowdhury, S. H. (2022). Myths about Coronavirus : A Research Defense. Global Journal of Health Science, 14(2), 63–112. https://doi.org/10.5539/gjhs.v14n2p63
Miah, M. R., Hasan, M. M., Miah, M. M. U., Parisha, J. T., Alam, M. S., Sayok, A. K., Rahman, M. S., Sharif, M. A., & Uddin, M. B. (2023f). Innovative Policy to Enable Sustained Conserving of Forest Biodiversity. International Journal of Agriculture and Forestry, 13(1), 1–22. https://doi.org/10.5923/j.ijaf.20231301.01
Miah, M. R., Hasan, M. M., Parisa, J. T., Alam, M. S. E., Hossain, M. M., Akhtar, F., Begum, M., Sayok, A. K., Abdullah, F., Shamsuddin, M. A. S., Rahman, A. A. M. S., Alam, M. S., & Chowdhury, S. H. (2021g). Coronavirus : A Terrible Global Democracy. International Journal of Applied Sociology, 11(2), 46–82. https://doi.org/10.5923/j.ijas.20211102.02
Miah, M. R., Hasan, M. M., Parisa, J. T., Alam, M. S. E., Shahriar, C. S., Akhtar, F., Begum, M., Sayok, A. K., Abdullah, F., Shamsuddin, M. A. S., Rahman, A. A. M. S., Alam, M. S., Tabassum, T., Chowdhury, S. H., Sharif, M. A., Rahman, M. S., Uddin, M. B., Tamim, M. A. K., Nazim, A. Y. M., … Chowdhury, M. A. K. (2022b). Impact of Oscillated Wireless Sensor Networks to Initiate Cardiac Arrest. International Journal of Internal Medicine, 11(1), 1–17. https://doi.org/10.5923/j.ijim.20221101.01
Miah, M. R., Hasan, M. M., Parisa, J. T., Alam, M. S., Akhtar, F., Begum, M., Shahriar, C. S., Sayok, A. K., Abdullah, F., Shamsuddin, M. A. S., Rahman, M. S., Sharif, M. A., Rahman, A. A. M. S., Alam, M. S., Uddin, M. B., & Chowdhury, S. H. (2021h). Unexpected Effects of Advanced Wireless Sensor Technology on Climate Change. World Environment, 11(2), 41–82. https://doi.org/10.5923/j.env.20211102.01
Miah, M. R., Hasan, M. M., Parisha, J. T., & Chowdhury, S. H. (2022a). Socioeconomic Impact of the Coronavirus Pandemic with Multiple Factors on Global Healthcare Policy. Journal of Politics and Law, 15(4), 242–253. https://doi.org/10.5539/jpl.v15n4p242
Miah, M. R., Hasan, M. M., Parisha, J. T., Chowdhury, S. H., & (et al.) Chowdhury, S. H. (2022g). Towards the Misuse of Advanced Wireless Sensor Technology to Enable the Sudden Onset of ARDS. American Journal of Medicine and Medical Sciences, 12(6), 616–638. https://doi.org/10.5923/j.ajmms.20221206.05
Miah, M. R., Hasan, M. M., Parisha, J. T., Chowdhury, S. H., & Sayok, A. K. (2023k). Misuse of Technology to Exacerbate Democracy in Crisis. American Journal of Sociological Research, 13(1), 12–23. https://doi.org/10.5923/j.sociology.20231301.03
Miah, M. R., Hasan, M. M., Parisha, J. T., Chowdhury, S. H., & Sayok, A. K. (2023). Misuse of Technology to Exacerbate Democracy in Crisis. American Journal of Sociological Research, 13(1), 12–23. https://doi.org/10.5923/j.sociology.20231301.03
Miah, M. R., Hasan, M. M., Parisha, J. T., Chowdhury, S. H., Sayok, A. K., & Uddin, M. B. (2023). A Unique Revolutionary Journey Across the Globe to Discover the Novel Coronavirus. International Journal of Research–Granthaalayah, 11(4), 84–100. https://doi.org/10.29121/granthaalayah.v11.i4.2023.5137
Miah, M. R., Hasan, M. M., Parisha, J. T., Huda, M. B., Sher-E-Alam, M., Kiew Sayok, A., Rahman, M. S., Sharif, M. A., Uddin, M. B., Chowdhury, S. H., & Bhuiyan, M. A. (2023). Misuse of Advanced Satellite Technology to Accelerate Man-Made Flash Floods. International Journal of Research–Granthaalayah, 11(3), 160–171. https://doi.org/10.29121/granthaalayah.v11.i3.2023.5058
Miah, M. R., Hasan, M. M., Parisha, J. T., Sayok, A. K., Alam, M. S., & Chowdhury, S. H. (2022h). Issues and Challenges in Medical Jurisprudence Due to Misuse of Wireless Sensor Technology. American Journal of Medicine and Medical Sciences, 12(12), 1277–1291. https://doi.org/10.5923/j.ajmms.20221212.23
Miah, M. R., Hasan, M. M., Parisha, J. T., Sayok, A. K., Uddin, M. B., Chowdhury, S. H., & Miah, M. M. U. (2023a). Impact of High radio frequency satellite oscillations on initiating earthquakes. International Journal of Research–Granthaalayah, 11(5), 129–197. https://doi.org/10.29121/granthaalayah.v11.i5.2023.5142
Miah, M. R., Hasan, M. M., Parisha, J. T., Shahriar, C. S., Sayok, A. K., & Chowdhury, S. H. (2022i). Adverse Global Health Impacts due to the Proliferation of Man-Made Technological Heatwaves. Resources and Environment, 12(3), 67–75. https://doi.org/10.5923/j.re.20221203.01
Miah, M. R., Hasan, M. M., Parisha, J. T., Shahriar, C. S., Sayok, A. K., Selim, M. A., & Chowdhury, S. H. (2023m). A Scientific Innovative Approach to Recovery from Dengue Fever. Public Health Research, 13(1), 1–14. https://doi.org/10.5923/j.phr.20231301.01
Miah, M. R., Hasan, M. M., Reza, M. S., Parisha, J. T., Shahriar, C. S., Rashid, M. M., Chowdhury, S. H., Malik, S. U. F., Azad, M. K. H., Samdany, A. A., Hossain, S. A. M. I., Sayok, A. K., Uddin, M. B., Miah, M. M. U., Naher, M. Q., Alam, M. S., Khatun, H., Chowdhury, M. A. K., Hossain, M. M., Habib, A., Nazim, A. Y. M., Chowdhury, M. A. A., & Uddin, M. M. (in press). Mysterious post-COVID with GPS Sensor Technology to Exacerbate Long-Term Global Crisis. International Journal of Engineering Technologies and Management Research.
Miah, M. R., Khan, M. S., Rahman, A. A. M. S., Samdany, A. A., Hannan, M. A., Chowdhury, S. H., & Sayok, A. K. (2020a). Impact of Sensor Networks Towards Individuals Augmenting Causes of Diabetes. International Journal of Diabetes Research, 9(2), 1–10. https://doi.org/10.5923/j.diabetes.20200902
Miah, M. R., Rahman, A. A. M. S., Hasan, M. M., Parisa, J. T., Hannan, M. A., Hossain, M. M., Alam, M. S., Alam, M. S. E., Akhtar, F., Ghani, M. A., Khan, M. S., Shahriar, C. S., Sayok, A. K., Begum, M., Malik, S. U. F., Samdany, A. A., Ahmed, G., & Chowdhury, S. H. (2021c). Adverse Effects of Wireless Sensor Technology to Debilitating in Numbness. International Journal of Virology and Molecular Biology, 10(1), 12–25. https://doi.org/10.5923/j.ijvmb.20211001.03
Miah, M. R., Rahman, A. A. M. S., Khan, M. S., Hannan, M. A., Hossain, M. S., Shahriar, C. S., Hossain, S. A. M. I., Talukdar, M. T. H., Samdany, A. A., Alam, M. S., Uddin, M. B., Sayok, A. K., & Chowdhury, S. H. (2021a). Effect of Coronavirus Worldwide Through Misusing of Wireless Sensor Networks. American Journal of Bioinformatics Research, 11(1), 1–31. https://doi.org/10.5923/j.bioinformatics.20211101.01
Miah, M. R., Rahman, A. A. M. S., Khan, M. S., Samdany, A. A., Hannan, M. A., Chowdhury, S. H., & Sayok, A. K. (2020). Impact of Sensor Technology Enhancing Corona Disease. American Journal of Biomedical Engineering, 10(1), 16–26. https://doi.org/10.5923/j.ajbe.20201002
Miah, M. R., Rahman, A. A. M. S., Parisa, J. T., Hannan, M. A., Khan, M. S., Samdany, A. A., Sayok, A. K., & Chowdhury, S. H. (2021d). Discovery of Coronavirus With Innovative Technology. Science and Technology, 11(1), 7–29. https://doi.org/10.5923/j.scit.20211101.02
Miah, M. R., Rahman, A. A. M. S., Samdany, A. A., & Chowdhury, S. H. (2021e). A Dynamic Scientific Model for Recovery of Corona Disease. Frontiers in Science, 11(1), 1–17. https://doi.org/10.5923/j.fs.20211101.01
Miah, M. R., Rahman, A. A. M. S., Sayok, A. K., Samdany, A. A., & Hannan, M. A. (2021). How to Fight the COVID-19 Global Crisis. World Journal of Environmental Research, 11(2), 31–38. https://doi.org/10.18844/wjer.v11i2.5855
Miah, M. R., Uddin, M. M., Parisha, J. T., Shahriar, C. S., Alam, M. S., Chowdhury, S. H., Nazim, A. Y. M., Hannan, M. A., Uddin, M. J., Uddin, M. B., Nipa, N. S., Khan, M. S., Ahmed, G., Hossain, M. S., Rashid, M. M., Samdany, A. A., Hossain, S. A. M. I., Selim, M. A., Uddin, M. F., … Chowdhury, M. T. R. (2023n). Uncontrolled Advanced Wireless Sensor Technology to Enable Early Growth of Stomach Cancer. American Journal of Stem Cell Research, 5(1), 8–39. https://doi.org/10.5923/j.ajscr.20230501.02
Mishra, C., & Meyer, J. J. (2022, November 7). Neovascular Glaucoma. In StatPearls. StatPearls Publishing.
Musch, D. C., Sugar, A., & Meyer, R. F. (1983). Demographic and Predisposing Factors in Corneal Ulceration. Archives of Ophthalmology, 101(10), 1545–1548. https://doi.org/10.1001/archopht.1983.01040020547007
Nguyen, D. D., Lue, S. J., & Lai, J. Y. (2021). Tailoring Therapeutic Properties of Silver Nanoparticles for Effective Bacterial Keratitis Treatment. Colloids and Surfaces B : Biointerfaces, 205, 111856. https://doi.org/10.1016/j.colsurfb.2021.111856
Pakzad-Vaezi, K., Levasseur, S. D., Schendel, S., Mark, S., Mathias, R., Roscoe, D., & Holland, S. P. (2015). The Corneal Ulcer One-Touch Study: A Simplified Microbiological Specimen Collection Method. American Journal of Ophthalmology, 159(1), 37–43.e1. https://doi.org/10.1016/j.ajo.2014.09.021
Ray, K. J., Prajna, L., Srinivasan, M., Geetha, M., Karpagam, R., Glidden, D., Oldenburg, C. E., Sun, C. Q., McLeod, S. D., Acharya, N. R., & Lietman, T. M. (2013). Fluoroquinolone Treatment and Susceptibility of Isolates from Bacterial Keratitis. JAMA Ophthalmology, 131(3), 310–313. https://doi.org/10.1001/jamaophthalmol.2013.1718
Reza, M. S., Chowdhury, S. A., Talukder, P. K., Islam, M. T., Hossain, M. A., Hussain, N. J., & Jhuma, A. A. (2021). Non-Viral Microbial Keratitis in a Tertiary Care Hospital in Bangladesh. Medicine Today, 33(2), 133–137. https://doi.org/10.3329/medtoday.v33i2.56059
Reza, M. S., Miah, M. R., Chowdhury, F. T., & Chowdhury, M. A. K. (2023a). Common Disease Profiles of Outpatients in Ophthalmology Department of Tertiary Care Hospital. International Journal of Optics and Applications, 9(1), 22–30. https://doi.org/10.5923/j.optics.20230901.02
Reza, M. S., Miah, M. R., Hussain, N. J., Chowdhury, F. T., Jhuma, A. A., & Hossain, M. A. (2023). Excision of the Pterygium with Conjunctival Autograft and Autologous Blood to Prevent Recurrence. American Journal of Medicine and Medical Sciences, 13(11), 1760–1777. https://doi.org/10.5923/j.ajmms.20231311.36
Robaei, D., & Watson, S. (2014). Corneal Blindness: A Global Problem. Clinical & Experimental Ophthalmology, 42(3), 213–214. https://doi.org/10.1111/ceo.12330
Sakr, S. I., Nayel, A. A., Habeel, C. S., Elkhabiry, H. K., Ibrahim, G. M., Tolba, M. M., & Ghaith, A. A. (2023). Epidemiological Profile of Microbial Keratitis in Alexandria, Egypt: A 5-Year Retrospective Study. Journal of Ophthalmic Inflammation and Infection, 13, 18. https://doi.org/10.1186/s12348-023-00332-7
Sand, D., She, R., Shulman, I. A., Chen, D. S., Schur, M., & Hsu, H. Y. (2015). Microbial Keratitis in Los Angeles : The Doheny Eye Institute and the Los Angeles County Hospital experience. Ophthalmology, 122(5), 918–924. https://doi.org/10.1016/j.ophtha.2014.11.027
Schaefer, F., Bruttin, O., Zografos, L., & Guex-Crosier, Y. (2001). Bacterial Keratitis: A Prospective Clinical and Microbiological Study. British Journal of Ophthalmology, 85(7), 842–847. https://doi.org/10.1136/bjo.85.7.842
Shoja, M. R., & Manaviat, M. (2004). Epidemiology and Outcome of Corneal Ulcers in Yazd Shahid Sadoughi Hospital. Acta Medica Iranica, 42, 136–141.
Solanki, S., Rathi, M., Khanduja, S., Dhull, C. S., Sachdeva, S., & Phogat, J. (2015). Recent trends : Medical Management of Infectious Keratitis. Oman Journal of Ophthalmology, 8(2), 83–85. https://doi.org/10.4103/0974-620X.159104
Soleimani, M., Cheraqpour, K., Sadeghi, R., Pezeshgi, S., Koganti, R., & Djalilian, A. R. (2023). Artificial Intelligence and Infectious Keratitis: Where Are We Now? Life, 13(11), 2117. https://doi.org/10.3390/life13112117
Soleimani, M., Masoumi, A., Khodavaisy, S., Heidari, M., Haydar, A. A., & Izadi, A. (2020). Current Diagnostic Tools and Management Modalities of Nocardia keratitis. Journal of Ophthalmic Inflammation and Infection, 10(1), 36. https://doi.org/10.1186/s12348-020-00228-w
Stellwagen, A., MacGregor, C., Kung, R., Konstantopoulos, A., & Hossain, P. (2020). Personal Hygiene Risk Factors For Contact Lens-Related Microbial Keratitis. BMJ Open Ophthalmology, 5(1), e000476. https://doi.org/10.1136/bmjophth-2020-000476
Truong, D. T., Bui, M. T., Memon, P., & Cavanagh, H. D. (2015). Microbial Keratitis at an Urban Public Hospital : A 10-year Update. Journal of Clinical & Experimental Ophthalmology, 6(6), Article 1000498. https://doi.org/10.4172/2155-9570.1000498
Ung, L., Bispo, P. J. M., Shanbhag, S. S., Gilmore, M. S., & Chodosh, J. (2019). The Persistent Dilemma of Microbial Keratitis: Global Burden, Diagnosis, and Antimicrobial Resistance. Survey of Ophthalmology, 64(3), 255–271. https://doi.org/10.1016/j.survophthal.2018.12.003
Upadhyay, M. P., Srinivasan, M., & Whitcher, J. P. (2015). Diagnosing and Managing Microbial Keratitis. Community Eye Health, 28(89), 3–6.
Vajpayee, R. B., Dada, T., Saxena, R., Vajpayee, M., Taylor, H. R., Venkatesh, P., et al. (2000). Study of the First Contact Management Profile of Cases of Infectious Keratitis: A Hospital-Based Study. Cornea, 19(1), 52–56. https://doi.org/10.1097/00003226-200001000-00011
Vemuganti, G. K., Murthy, S. I., & Das, S. (2011). Update on Pathologic Diagnosis of Corneal Infections and Inflammations. Middle East African Journal of Ophthalmology, 18(4), 277–284. https://doi.org/10.4103/0974-9233.90128
Wen, S., Qin, C., Shen, L., Liu, D., Zhu, S., & Lin, Q. (2022). Surface Self-Assembly Construction of Therapeutic Contact Lens with Bacterial “Kill-Releasing” and Drug-Reloading Capabilities for Efficient Bacterial Keratitis Treatment. ACS Biomaterials Science & Engineering, 8(3), 1329–1341. https://doi.org/10.1021/acsbiomaterials.1c01557
Willcox, M. (2007). Pseudomonas Aeruginosa Infection and Inflammation During Contact Lens Wear : A Review. Optometry and Vision Science, 84, 273–278. https://doi.org/10.1097/OPX.0b013e3180439c3e
Wong, R. L., Gangwani, R. A., Yu, L. W., & Lai, J. S. (2012). New Treatments for Bacterial Keratitis. Journal of Ophthalmology, 2012, 831502. https://doi.org/10.1155/2012/831502
Yang, J. W., Song, Q. Y., Zhang, M. X., Ai, J. L., Wang, F., Kan, G. H., Wu, B., & Zhu, S. Q. (2022). Spaceflight-Associated Neuro-Ocular Syndrome : A Review of Potential Pathogenesis and Intervention. International Journal of Ophthalmology, 15(2), 336–341. https://doi.org/10.18240/ijo.2022.02.21
Young, A. L., Leung, K. S., Tsim, N., Hui, M., & Jhanji, V. (2013). Risk Factors, Microbiological Profile, and Treatment Outcomes of Pediatric Microbial Keratitis in a Tertiary Care Hospital in Hong Kong. American Journal of Ophthalmology, 156(5), 1040–1044.e2. https://doi.org/10.1016/j.ajo.2013.06.019
Younger, J. R., Johnson, R. D., Holland, G. N., Page, J. P., Nepomuceno, R. L., Glasgow, B. J., Aldave, A. J., Yu, F., Litak, J., Mondino, B. J., & UCLA Cornea Service. (2012). Microbiologic and Histopathologic Assessment of Corneal Biopsies in the Evaluation of Microbial Keratitis. American Journal of Ophthalmology, 154(3), 512–519.e2. https://doi.org/10.1016/j.ajo.2012.03.014
Zemba, M., Stamate, A. C., Tataru, C. P., Branisteanu, D. C., & Balta, F. (2020). Conjunctival Flap Surgery in the Management Of Ocular Surface Disease: Review. Experimental And Therapeutic Medicine, 20(4), 3412–3416. https://doi.org/10.3892/etm.2020.8964
Zhai, Y., Pang, C., Sun, S., Ma, O., Han, L., Gu, Y., & Gu, L. (2021). A Case Report of Gemella Haemolysans Keratitis After Refractive Surgery. Infection and Drug Resistance, 14, 5175–5181. https://doi.org/10.2147/IDR.S339018
Zhou, Y., Sharifi, A., Gupta, P., Duong, B., Lahiji, A. P., He, J., & Lee, W. H. (2022). Vision Loss as Presenting Symptom in Testicular Cancer : A Morbid Case Report. Case Reports in Ophthalmology, 13(3), 756–762. https://doi.org/10.1159/000526748
 This work is licensed under a: Creative Commons Attribution 4.0 International License
This work is licensed under a: Creative Commons Attribution 4.0 International License
© Granthaalayah 2014-2025. All Rights Reserved.