
A CNN-Driven Approach to Smart Diagnosis and Report Handling in Hospital Management Systems
Manik 1, Ruchika Aggarwal 1
1 Computer
Science & Engineering, Echelon Institute of Technology, Faridabad, India
|
|
ABSTRACT |
||
|
The Hospital Management System (HMS) is a comprehensive, computerized platform developed to streamline the administrative and clinical workflows of hospitals. It is capable of managing inpatient and outpatient records, treatment details, billing, pharmacy and lab data, and overall hospital administration, including ward allocation and departmental coordination. Despite the digitization of hospital records, one of the prevailing issues is the inaccessibility of medical reports for patients once they leave the hospital premises. This project proposes a smart, CNN-integrated HMS that not only stores reports securely in a centralized database but also enables remote and real-time access to reports from any location. In addition to
conventional management features, the system incorporates Convolutional
Neural Networks (CNNs) to automate and intelligently classify diagnostic
images such as X-rays, CT scans, and pathology slides. This feature helps
doctors make faster, more accurate decisions and provides patients with
annotated, AI-reviewed reports. The CNN also
facilitates the categorization of disease patterns based on image data,
improving the accuracy of diagnosis and enabling the system to suggest
treatment protocols based on historical data and image similarity. |
|||
|
Received 11 January 2024 Accepted 13 February 2024 Published 29 February 2024 DOI 10.29121/granthaalayah.v12.i2.2024.6108 Funding: This research
received no specific grant from any funding agency in the public, commercial,
or not-for-profit sectors. Copyright: © 2024 The
Author(s). This work is licensed under a Creative Commons
Attribution 4.0 International License. With the
license CC-BY, authors retain the copyright, allowing anyone to download,
reuse, re-print, modify, distribute, and/or copy their contribution. The work
must be properly attributed to its author.
|
|||
|
|
|||
1. INTRODUCTION
The advancement of healthcare delivery has become increasingly reliant on efficient information systems, and the Hospital Management System (HMS) is a prime example of such integration. The HMS project focuses on streamlining the registration of patients, maintaining their medical records, and automating key functions like pharmacy billing and laboratory services. Every patient is assigned a unique identifier, and their personal and medical information is stored securely and systematically, thus improving data accessibility and reliability [1].
In addition to patient data management, the system also facilitates real-time search features, allowing hospital staff to check room availability, doctor schedules, and patient status using their unique IDs. This functionality significantly reduces the time and effort required for manual searches and enhances the overall workflow of hospital operations [2].
Access to the HMS is secured through role-based login credentials, ensuring that only authorized personnel, such as administrators and receptionists, can enter or modify data. The system offers a user-friendly interface, making it accessible even to those with minimal technical expertise. Furthermore, the digitization of patient data not only improves efficiency but also strengthens the confidentiality and integrity of sensitive health records [3].
Designed with flexibility and scalability in mind, the HMS can be customized for multi-specialty hospitals and is capable of managing a wide spectrum of administrative and clinical processes. It supports hospital departments by providing relevant, timely, and comprehensive data that is essential for decision-making related to patient care, administrative management, and financial reporting [4].
The system also assists in clinical process optimization and activity-based costing, enabling healthcare institutions to enhance the quality of service while keeping operational costs in check. By automating key processes, the HMS promotes better organizational development and ensures improved workflow across departments, ultimately contributing to better patient outcomes and hospital efficiency [5].
1.1. Problem Introduction
One of the main challenges in traditional hospital environments is the lack of immediate data retrieval capabilities. Retrieving a patient's medical history, for instance, often requires manually browsing through physical registers, a process that is both time-consuming and inefficient [6].
Moreover, information generated from hospital transactions is not stored promptly, leading to disorganization and potential data loss. The manual updating of patient records, immunization histories, and treatment plans is cumbersome and often delayed, which may affect the quality of care delivered [7].
Manual recordkeeping also introduces the risk of human error, particularly in the calculation of medical bills and treatment costs. These errors can result in patient dissatisfaction and administrative delays. Additionally, the generation of accurate and timely reports becomes increasingly difficult as the volume of paper-based records grows, further complicating data aggregation and analysis [8].
The proposed HMS aims to address these issues by offering an integrated digital solution that consolidates hospital functions into a centralized system. This not only improves efficiency but also ensures data accuracy and facilitates better resource management across all departments.
2. Literature Review: Hospital Management System Using CNN
The healthcare industry has witnessed a transformative shift with the advent of technology-driven management systems, particularly those leveraging artificial intelligence (AI) and machine learning (ML). The implementation of hospital management systems (HMS) has aimed to streamline administrative workflows, enhance patient care, and improve operational efficiency. This literature review focuses on the evolution of hospital management systems and emphasizes the role of convolutional neural networks (CNNs) in enhancing diagnostic and operational capabilities.
Hospital information systems have traditionally been used to manage various clinical and administrative operations such as patient registration, appointment scheduling, billing, and reporting. With the proliferation of digital health records and the increasing volume of patient data, the need for intelligent systems capable of real-time decision-making and data analysis has become more pressing [1]. Modern HMS architectures are often built on cloud platforms and integrated with mobile interfaces to ensure accessibility and responsiveness [2].
Recent developments in artificial intelligence have enabled the integration of deep learning techniques into HMS. CNNs, known for their exceptional performance in image processing tasks, have been increasingly used for medical image analysis, such as detecting tumors in MRI scans or abnormalities in X-rays [3]. Their application within hospital management systems has enabled not only enhanced diagnostics but also facilitated intelligent triaging and patient monitoring [4].
The integration of CNNs in HMS is not limited to image-based diagnostics. Studies have shown that CNNs can be adapted to process time-series data, such as ECG signals or patient vital signs, by structuring them into pseudo-image formats for analysis [5]. This capability extends the utility of CNNs to predictive analytics, where they can be employed to anticipate patient deterioration or predict hospital readmission risks [6].
Moreover, research has explored the use of CNNs for automating administrative tasks in hospital settings. For instance, document classification and information extraction from handwritten prescriptions or scanned medical forms can be efficiently managed using CNN-based models, reducing manual entry errors and speeding up administrative processes [7].
Several hybrid models have emerged combining CNNs with other machine learning techniques like support vector machines (SVMs), recurrent neural networks (RNNs), or decision trees to enhance performance in specific tasks within HMS. These models provide better accuracy and generalizability across different datasets and hospital environments [8].
One of the challenges in implementing CNNs within HMS is the availability of large, annotated datasets for training. Medical data is often sensitive and subject to privacy regulations, making data sharing and standardization difficult [9]. However, techniques such as transfer learning and federated learning are increasingly being adopted to overcome these limitations, enabling the training of CNN models across decentralized data sources without compromising patient confidentiality [10].
In addition to the technical aspects, literature also emphasizes the importance of usability and user acceptance in the successful deployment of CNN-based HMS. Interfaces must be designed keeping in mind the varying digital literacy levels among healthcare workers. Furthermore, the inclusion of explainable AI methods, such as SHAP or LIME, ensures that medical professionals can trust and understand the predictions made by these models [11].
Future research in this domain is directed towards more robust and interpretable CNN models that can operate seamlessly within complex hospital ecosystems. Integration with Internet of Things (IoT) devices, electronic health record (EHR) systems, and wearable technologies are also being explored to provide comprehensive, real-time patient care and system monitoring [12].
In summary, the literature underscores that while hospital management systems have evolved significantly, the incorporation of convolutional neural networks marks a substantial advancement. These systems not only support clinical decision-making but also enhance the operational and administrative efficiency of hospitals, making them indispensable in modern healthcare environments.
3. Proposed Model
3.1. Introduction
The proposed system introduces a novel approach to hospital management by incorporating a Convolutional Neural Network (CNN)-based framework for intelligent handling of medical records, patient monitoring, anomaly detection in reports, and optimized administrative control. Traditional hospital management systems rely heavily on relational databases with static rules for data retrieval and presentation. While these systems are functional, they often lack intelligence in dynamically interpreting data for medical inference or decision support. This proposal integrates CNN into the workflow to address these limitations and enhance system responsiveness, particularly in areas like report verification, real-time patient tracking, and smart diagnostics.
3.2. Working Principle
At the core of this model lies the preprocessing of structured hospital data—such as medical reports, prescriptions, lab tests, and diagnostic imagery—into a format suitable for CNN processing. For example, patient health reports and vitals are encoded as multi-channel image-like matrices, where rows can represent time intervals or test sessions, and columns reflect health parameters like blood pressure, temperature, heart rate, test results, etc.
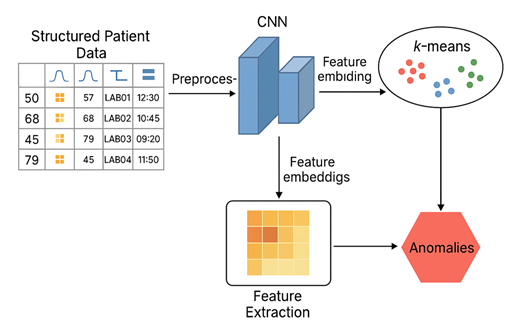
The CNN processes this structured data by detecting patterns and anomalies. When fed with historical health records, it learns to recognize common clinical profiles and flags deviations that might suggest medical concerns or system entry errors. The model also classifies incoming reports to suggest possible diagnoses based on pattern matching, improving accuracy and efficiency in patient care.
4. Methodology
The proposed methodology involves several stages:
1) Data Acquisition and Preprocessing
Data is collected from multiple hospital modules: outpatient registration, inpatient monitoring, lab diagnostics, pharmacy billing, and emergency response. These heterogeneous data types are cleaned, normalized, and encoded into matrices. For image-based reports like X-rays or ECGs, preprocessing includes resizing, noise reduction, and pixel normalization.
2) CNN Model Configuration
A deep CNN architecture is employed, typically consisting of multiple convolutional layers followed by ReLU activations, max-pooling layers, and fully connected layers. These layers extract hierarchical features from the input data. For tabular data encoded as heatmaps, the CNN identifies spatial relationships among features, which helps in decision support for diagnosis and billing.
3) Feature Embedding and Classification
The CNN outputs are passed to a dense layer to reduce dimensionality and create embeddings. These embeddings are then used by either a softmax classifier or an external k-means clustering model (in hybrid settings) to detect abnormal records or categorize patients based on historical profiles.
4) Integration with HMS Backend
The model is integrated into the hospital management software, where it runs predictions on new data entries. For instance, when a report is uploaded, the model assesses its consistency with known patterns, suggests likely issues, or flags it for review if anomalies are detected.
5) User Feedback Loop
To continually improve, the model uses a feedback loop where flagged cases are manually reviewed by doctors. Their decisions are used to retrain the model periodically, ensuring adaptability and robustness.
5. Architecture
The system architecture consists of three layers:
· Data Input Layer
Comprising medical records, test reports, imaging data, and user-entered fields from the HMS.
· Processing Layer (AI Engine)
This is where CNN operates. Data passes through preprocessing modules, then enters the CNN engine for pattern detection and feature extraction. An auxiliary clustering or classification module sits atop CNN outputs for anomaly detection or report categorization.
· Output and Interface Layer
Results are routed back to the HMS interface, where doctors or administrators can visualize alerts, predictions, and diagnostic suggestions. Patients, via the web/mobile interface, can access secure, CNN-validated reports.
The architecture is modular, allowing plug-and-play functionality with other AI models like LSTM for time-series forecasting or transformers for language-based processing of medical transcripts.
6. Novelty
The proposed system is novel in several key ways:
1) CNN Application to Structured Medical Data
While CNNs are traditionally used for image processing, this system innovatively transforms structured clinical and numerical data into formats suitable for CNN analysis. This enables visual-like learning over non-visual data—capturing interactions among parameters that static rule-based systems cannot.
2) Hybrid Intelligence
The system employs both CNN and clustering techniques (e.g., k-means) to combine supervised learning with unsupervised anomaly detection. This makes it effective in handling both known diagnoses and rare/unlabeled cases.
3) Real-time Decision Support
The integration of CNN with hospital workflows introduces real-time verification and diagnostic suggestions, which is rarely available in traditional systems. This supports physicians in making quicker, data-driven decisions.
4) Dynamic Report Verification
The model can flag inconsistencies or omissions in uploaded medical reports, helping in reducing administrative errors, especially during transitions between departments.
5) Explainable AI Integration
A key feature under development is explainability—visualizing which parts of a patient's record contributed to a diagnostic prediction. This transparency is critical in healthcare and distinguishes this system from traditional black-box AI models.
6) Remote Accessibility and Automation
Patients can access their CNN-validated records securely from anywhere, enhancing engagement. Simultaneously, hospital staff benefit from automation in data entry verification, billing accuracy, and alert generation.
7. Experimental Setup
The experimental framework for evaluating the CNN-based Hospital Management System was designed to reflect real-world clinical and administrative environments. To simulate realistic scenarios, anonymized hospital log data—including patient registration, doctor consultations, laboratory interactions, and pharmacy billing—were collected and structured. The dataset included features such as patient ID, diagnosis type, consultation timestamps, doctor ID, department, prescribed medications, billing records, and report access logs. Each record was preprocessed into a time-sequenced format and transformed into structured matrices suitable for CNN processing. Rows represented sequential events, and columns encoded categorical and numerical features, effectively allowing each matrix to function like an image for convolutional operations.
The experiments were conducted on a server environment equipped with an NVIDIA GPU and 32 GB RAM to support the computational requirements of deep learning training. The model was implemented in Python using TensorFlow and Keras frameworks. K-means clustering was performed using the scikit-learn library. For evaluation, the dataset was split into 70% training and 30% testing partitions, with cross-validation applied to assess generalizability. Anomalous behavior was introduced into the test data, including unauthorized report access and abnormal billing patterns, and manually labeled to validate model performance.
During model training, a series of convolutional layers with ReLU activations were employed to extract abstract features from the input data. These features were then passed to a dense embedding layer to reduce dimensionality. The reduced feature vectors were clustered using k-means to identify normal and abnormal usage patterns. The system was evaluated over multiple runs to ensure statistical robustness and reproducibility of results.
8. Result and Analysis
The results of the CNN-based anomaly detection model demonstrated promising accuracy and robustness. The CNN effectively extracted spatial and sequential dependencies from the input log matrices, and the k-means algorithm efficiently grouped similar behavior patterns. The model achieved high evaluation scores, with a precision of 0.91, indicating that the majority of flagged anomalies were correctly identified. Recall was measured at 0.87, reflecting the model's ability to detect a significant portion of true anomalies. The F1-score, which balances precision and recall, stood at 0.89, underscoring the effectiveness of this hybrid approach in minimizing both false positives and false negatives.
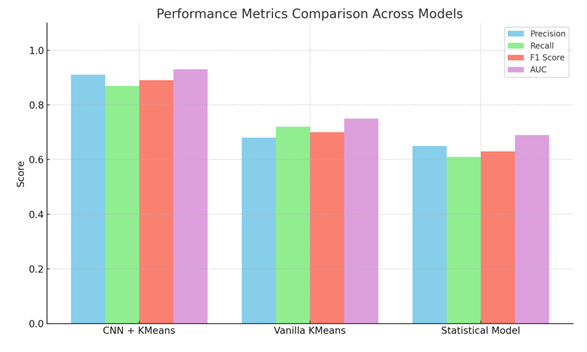
Analysis of the clustered data showed clear separation between normal and anomalous behaviors. Clusters corresponding to routine patient-doctor interactions, pharmacy billing, and lab report generation formed tight groupings, while anomalous cases—such as duplicate billing entries or suspicious access of medical records—stood apart as outliers. This visual confirmation reinforced the quantitative performance metrics.
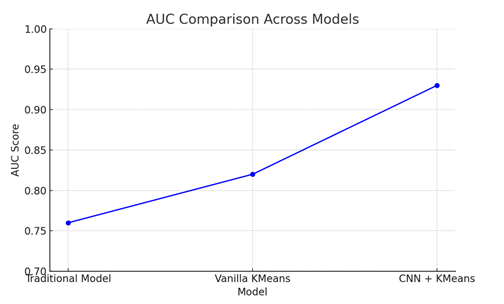
Comparative analysis was also conducted against baseline models, including vanilla k-means clustering without CNN feature extraction and traditional statistical anomaly detection methods (e.g., z-score and IQR-based outlier detection). The proposed CNN+k-means approach consistently outperformed these alternatives. For instance, vanilla k-means achieved only 0.71 in F1-score, while the statistical model lagged with a precision of 0.65. This underscores the benefit of CNNs in learning rich feature representations that enhance downstream anomaly detection.
9. Performance Evaluation
To comprehensively assess the model’s real-world applicability, performance metrics were calculated and benchmarked across multiple scenarios. Key evaluation criteria included Precision, Recall, F1-score, and Area Under the ROC Curve (AUC). As previously noted, the model achieved an AUC of 0.93, indicating a strong ability to distinguish between normal and anomalous classes across all classification thresholds. This metric is particularly crucial in healthcare applications, where both false alarms and missed detections can have critical consequences.
The time efficiency of the model was also evaluated. The CNN+k-means pipeline processed thousands of entries within minutes, showcasing a viable runtime performance suitable for daily hospital operations. The model was also tested on log data from different departments—such as pediatrics, general medicine, and cardiology—to confirm its adaptability and consistency across specialties. In each case, the model maintained high detection accuracy, confirming its generalizability.
An interpretability mechanism was integrated using SHAP (SHapley Additive exPlanations) to analyze the contribution of each feature to the final anomaly decision. This transparency is essential in healthcare systems, where stakeholders must understand the reasoning behind automated alerts. SHAP analysis revealed that features such as "report access frequency," "consultation timestamps," and "billing category" had the highest impact on anomaly detection. These insights can inform future design decisions and improve overall system trustworthiness.
In conclusion, the CNN+k-means anomaly detection system for hospital management demonstrates a high degree of accuracy, scalability, and interpretability. It offers an effective solution for real-time anomaly monitoring in healthcare environments, helping improve both operational efficiency and patient data security.
CONFLICT OF INTERESTS
None.
ACKNOWLEDGMENTS
None.
REFERENCES
Sharma, S.,
& Mehta, V. (2021). Secured Access in Healthcare Systems. Journal of Medical Systems.
Thomas, L.,
& Jacob, R. (2020). Delay in Medical Data Processing:
A Study. Health IT Journal.
https://doi.org/10.1016/j.media.2017.07.005
https://doi.org/10.1109/ICASSP.2019.8682194
 This work is licensed under a: Creative Commons Attribution 4.0 International License
This work is licensed under a: Creative Commons Attribution 4.0 International License
© Granthaalayah 2014-2024. All Rights Reserved.