
Digital Block Applications; A Detailed Survey Between Surgical Branch Specialist and Specialist Students
Ali Osman Taşova 1![]()
![]() ,
Mustafa Cem Sürecek 2
,
Mustafa Cem Sürecek 2![]()
![]()
1 M.D.
Çanakkkale Ezine State Hospital, Department of Orthopedics and Traumatology
Ezine/Çanakkkale, Turkey
2 M.D.
Iğdır Dr. Nevruz Erez State Hospital, Department of Anesthesia and
Reanimation, Iğdır, Turkey
|
|
ABSTRACT |
||
|
Purpose: The purpose of this study was to investigate the digital block application methods of specialists and assistants working in the Departments of Orthopedics and Traumatology, Emergency Medicine, Anesthesia and Reanimation, and Plastic and Reconstructive Surgery in Turkey and the accuracy of the information on which these methods are based, through a survey, and to interpret the survey results. Study plan: In the survey consisting of a total of eighteen questions, the personal information of the physicians, their preferred digital block application methods, local anesthetic agent selection and application doses, and the source of the information on which these preferences are based were questioned in a digital environment. The responses were interpreted and analyzed. Findings: A total of 110 physicians, 16 specialists and 94 assistants, participated in our survey. In the responses given to the multiple-choice question asked to the participants about the cases you encounter most frequently in your clinic, we saw that the most common ones were fractures at the finger and toe level, skin and subcutaneous lacerations at the finger level, and tendon injuries. In the responses we received to the question of the most preferred type of anesthesia in such injuries, we saw that 51.9% preferred digital block and 42.6% preferred regional anesthesia. In the responses we received to other questions regarding the application method, dosage and different usage patterns in our survey, it was seen that traditional and personal experiences were effective in digital block applications. Conclusion: It was determined that the digital nerve block applications
preferred by specialists and specialist students were not compatible with the
literature. The results of the study are warning signs for the revision of
digital block applications. Experience-based applications and personal
teachings should be replaced by evidence-based applications in digital block
applications. |
|||
|
Received 21 December 2024 Accepted 09 January
2025 Published 05 February 2025 Corresponding Author Ali osman
Taşova, atasova1@hotmail.com DOI 10.29121/granthaalayah.v13.i1.2025.5867 Funding: This research
received no specific grant from any funding agency in the public, commercial,
or not-for-profit sectors. Copyright: © 2025 The
Author(s). This work is licensed under a Creative Commons
Attribution 4.0 International License. With the
license CC-BY, authors retain the copyright, allowing anyone to download,
reuse, re-print, modify, distribute, and/or copy their contribution. The work
must be properly attributed to its author.
|
|||
|
Keywords: Digital Block, Guide, Survey |
|||
1. INTRODUCTION
Digital nerve block is a simple procedure that can be performed to provide immediate anesthesia for many injuries and procedures such as fractures, dislocations, laceration repair, nail removal or drainage of infections. It is one of the most commonly performed nerve blocks in the emergency department due to its wide variety of uses and efficacy Knoop et al. (1994). The digital block is used for minor surgical interventions on the fingers, with or without digital tourniquets, because the use of general anesthesia for such surgical procedures carries greater risks, is often unnecessary, and is much more expensive. Digital nerve block is generally superior to local infiltration due to the reduced amount of anesthetic required. This is important as only a limited amount of anesthetic is tolerated in the limited area of the fingers De Buck et al. (2012).
Digital anesthetic blocks basically consist of local anesthetic deposition around nerves; For this purpose, first of all, important regional anatomical details should be well known. Digital nerve blocks are intended to numb the specific nerves originating from the deep branches of the median, radial and ulnar nerves at the wrist level. The dorsal nerve set travels alongside it at the 10 and 2 o'clock positions, while the palmar nerve set travels at the 4 and 8 o'clock positions. Each finger is innervated by four digital nerves. All four nerves must be blocked to achieve a full anesthetic effect. The palmar (or volar) digital nerves of the fingers arise from the median or ulnar nerves and branch out into the palm. These nerves are accompanied by digital blood vessels as they travel on either side of the flexor tendon sheath to innervate each finger. Palmar nerves are dominant in the entire finger except the ridge and innervate the nail bed. Dorsal digital nerves running along the dorsolateral aspect of each finger innervate the dorsum of the finger.
The basic approach is the same for both toes and fingers. Various techniques have been described for anesthetizing the digits. These include the traditional four-sided "ring block," the three-sided digital block, the finger web space block, the transthecal block, and the subcutaneous block Morrison (1993),Hill et al. (1995)).
Regardless of the technique chosen, advance and inject slowly to minimize pain being caused by distension of the tissues from infiltration of the fluid. Avoid using more than 3 to 4 mL of anesthetic solution. The mechanical pressure effects of injecting solution into a potentially confined space should always be borne in mind, particularly in blocks at the base of the digit.
The anesthetic choice should be tailored to the length of the desired analgesia. The most commonly used anesthetics are lidocaine (1.5-2 hours), lidocaine with epinephrine (2-6 hours), bupivacaine (2-4 hours), and mepivacaine (3-5 hours). Recommended dosage recommendations for commonly used local anesthetic agents are given in Table 1 (Dadure et al. (2015),American Academy of Pediatrics, & American Academy of Pediatric Dentistry; Cote, C. J., Wilson, S., & Sedation Working Group. (2006)).
Table 1
|
Table 1 Dosage Recommendations are Given for Commonly used Local Anesthetic Agents. (5,6) |
||||
|
Local anesthesia |
Without epinephrine |
With epinephrine |
||
|
|
Maximum dose |
Maximum dose |
Maximum dose |
Maximum dose |
|
Bupivacaine |
2 mg/kg |
175 mg |
3 mg/kg |
225 mg |
|
Levobupivacaine |
2 mg/kg |
200 mg |
3 mg/kg |
225 mg |
|
lidocaine |
5 mg/kg |
350 mg |
7 mg/kg |
500 mg |
|
mepivacaine |
5 mg/kg |
350 mg |
7 mg/kg |
500 mg |
|
Ropivacaine |
3 mg/kg |
200 mg |
3 mg/kg |
250 mg |
|
Prilocaine |
6 mg/kg |
400 mg |
8 mg/kg |
600 mg |
Contraindications in digital block applications include dangerous digital circulation, infection of the skin or tissues through which the needle will pass, and patients allergic to the anesthetic agent. Other considerations include avoiding the use of epinephrine anesthetics in patients at risk of ischemic injury, considering other techniques if the neurological function of the finger has been compromised by a previous injury, using a small amount of anesthetic to reduce mechanical stress on nerves and blood vessels and avoiding direct injections into nerves.
Epinephrine causes local vasoconstriction, thereby reducing bleeding, and maintains the anesthetic in the tissues for a longer period of time. However, the digital arteries run in close proximity to the digital nerves and injecting epinephrine into the base of a digit causes vasoconstriction of these vessels Altınyazar et al. (2004) which may increase the risk of digital ischemia in susceptible individuals. Digital blocks are commonly taught to be performed without epinephrine due to the risk of vasoconstriction leading to distal necrosis. However, recent studies provide no evidence of this occurrence (Silva Neto et al. (2020),Mantilla-Rivas et al.).
Complications of digital nerve blocks include, but are not limited to infection, bleeding, increased pain, vascular injection of anesthetic, nerve injury including neuropraxia or neurolysis, local anesthetic systemic toxicity (LAST), and allergic reaction.
2. Methods
The questionnaire consisting of eighteen questions is given in Table 2 Institutional ethics committee (XXXX XXXXX Clinical Research Ethics Committee) permissions were obtained. The questions were prepared to collect information about the demographic profile of the participants, their current views on local anesthesia, local analgesia application methods, commonly used drugs, drug administration doses and complications. After the final draft questions, one-on-one to the specialists and specialty students working in the departments of Emergency medicine, Plastic and reconstructive surgery, Orthopedics and traumatology and Anesthesiology and Reanimation working in Turkey through the "Google Forms" website (docs.google.com/forms). sent via e-mail after contact. The questionnaire was re-sent to those who did not respond or partially responded at an interval of 3 weeks. At the end of two months, the survey was closed to receiving responses on the website. A total of 110 people participated in our survey across the country. Table 2
Table 2
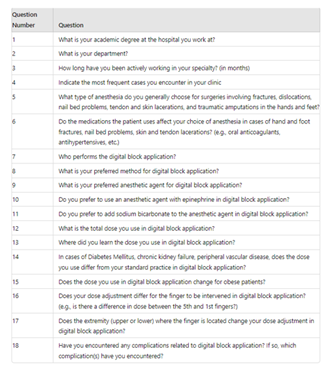
|
Table 2 Questionairre form Used |
Statistical analysis: In our survey study, numerical data was taken from the answers given to evaluate the general level of knowledge. We evaluated it with analytical approaches based on expert opinions. The answers received were analyzed with percentage values. Since there were no group comparisons in our study, no additional statistical analysis was performed.
3. Results
A total of 110 physicians, 16 specialists and 94 residents with academic degrees, participated in our survey. As for the branch distribution, there were 50 doctors from orthopedics and traumatology, 26 emergency medicine, 18 plastic and reconstructive surgery, and 16 anesthesia and reanimation departments.45.5% of the participants consisted of doctors who had worked in the profession for 3 years or more, while the number of people in their first year in the profession was 14.5% of the total number (Graph 1). In the answers given to the question of the most common cases in your multiple-choice clinic asked to the participants, we found that the most common fractures at the level of the fingers and toes, skin-subcutaneous incisions at the level of the fingers and tendon injuries. Again, we have seen that amputation from finger level and nail bed problems are encountered more rarely in clinics. We have seen that 51.9% digital block and 42.6% regional anesthesia were chosen in the answers we received to which anesthesia type is preferred by you, preferably for surgery in cases of fracture-dislocation, nail bed problems, tendon-skin cuts and traumatic amputation in the hand and foot. Although there was no choice of Bier-block anesthesia, 5.6% of the participants made the choice of general anesthesia primarily. It was observed that the drugs used by the patients were effective on the choice of anesthesia at a rate of 57.4% in case of finger and toe fractures, nail bed problems, skin and tendon cuts, and 42.6% thought that they did not affect the choice of anesthesia.
Graph 1
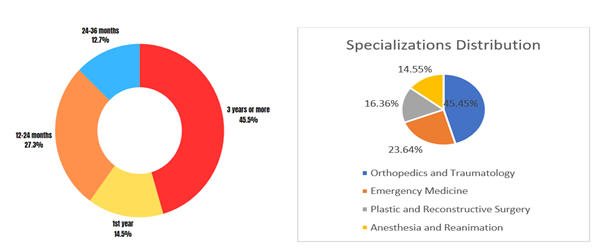
|
Graph 1 Profession experience and Distribution |
According to the results of the surveys we conducted in the clinics, it was observed that the application, which was performed by a senior assistant and a specialist, was generally preferred by experienced people (79.7%). We see that the majority of the participants use the traditional three-sided digital block application (49%) as the digital block application method and most frequently prefer prilocaine (61.1%) as the anesthetic agent. Among the application methods, 4-sided block applications (26.5%) and web spacing block (16.3%) were seen as other methods frequently preferred by the participants. Transthecal block is a method preferred by very few (8.2%) of the participants. Table 3
Table 3
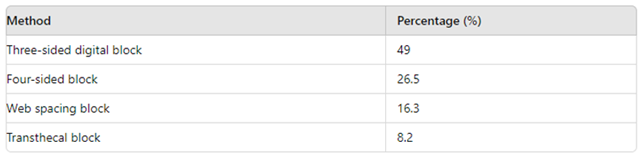
|
Table 3 Interviewers'
Answers to Digital Block Application Methods |
Prilocaine is the most preferred local anesthetic as an anesthetic agent, and the number of participants (5.6%) who used lidocaine + adrenaline as the first choice was found to be low. Table 4
Table 4
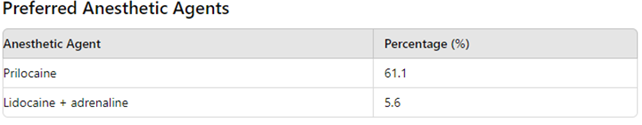
|
Table 4 Selection of Anesthetic Agent used by Interviewers for Digital
Block Application |
Again, we see that the majority of the participants prefer not to use epinephrine (83%) and bicarbonate (90.6%) in the digital block application. Table 5 The majority of the participants (49%) chose 2-4 mg/kg as the maximum dose option to be used. The proportion of participants choosing 0.5-1 mg/kg was 10.2%, 16.3% choosing a dose of 5 mg and above, and 24.5% choosing different dose administration. and the maximum dose for prilocaine is stated in the literature as 6 mg/kg. Table 6
Table 5
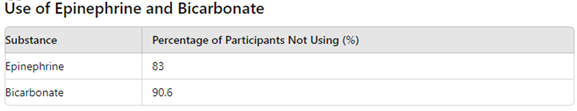
|
Table 5 Bicarbonate and Epinephrine usage Rates of Interviewees for Digital Block Application |
Table 6
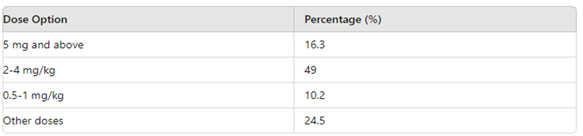
|
Table 6 Maximum Prilocaine usage doses of Interviewees for Digital Block Application |
We think that the other option is preferred at a high rate because the calculation of the anesthetic agent in grams cannot be made or is unknown, except for the low dose selection. In the question in which the source of the information about the dose was questioned, 69.2% of the participants chose the option that they learned from their senior, and 5.8% of the participants chose the option that they learned from an expert or lecturer. It was concluded that access to information from magazines and books was 15.6%, and learning from the Internet was chosen by only 9.4% of the participants.
Most of the participants (76.9%) stated that they would apply the dose they routinely apply in case of additional diseases such as diabetes mellitus, peripheral vascular disease and chronic kidney failure. Likewise, the majority of the participants (83%) were of the opinion that there was no reason for dose change in case the patient was obese.
Does your dose adjustment change for the finger to be intervened in the digital block application? (For example, is there a dose difference between the 5th finger and the 1st finger?), 62.3% of the participants replied that the dose did not change, while 37.7% of them replied that the dose used for each finger changed. The question with the closest results among the participants was the question of whether the dose to be applied in the lower and upper extremities changed. 58.5% of the participants answered that the dose did not change, and 41.5% of the participants answered that the dose should be changed.
In the last question of our survey, the complications they encountered with multiple choice were asked to the respondents, and it was seen that 77.9% of them did not face any complications. It was observed that the number of participants who encountered serious complications such as anaphylaxis, ischemia and LAST syndrome was very low.
4. Discussion
Digital nerve block is a simple procedure that can be performed to provide immediate anesthesia for many injuries and procedures such as fractures, dislocations, laceration repair, nail removal or drainage of infections. It is one of the most commonly performed nerve blocks in the emergency department due to its wide variety of uses and efficacy Knoop et al. (1994).
Our aim was to measure and evaluate the digital block application and knowledge levels of a total of 110 doctors who participated in our survey. The majority of our participants (85.5%) consisted of doctors who worked in the profession for more than 1 year. This participation shows us that questions are answered by physicians with a certain experience in the field. From the answers we received, it was thought that fractures at the level of the fingers and toes, skin-subcutaneous incisions at the level of the fingers and tendon injuries were frequently encountered in the clinics, so the participants had sufficient experience in the follow-up and treatment of this group of patients.
We have seen that 51.9% digital block and 42.6% regional anesthesia were chosen in the answers we received to the general anesthesia type question, which is preferred by you, preferably for surgery in cases of fracture-dislocation, nail bed problems, tendon-skin cuts and traumatic amputation in the hand and foot. The majority of the participants thought that the problem could be solved by using regional anesthesia regardless of the drugs used by the patient. It also leads to the conclusion that the digital block application is made by senior people in the clinics and that certain experience and knowledge are required
The basic approach is the same for both toes and fingers. Various techniques have been described for anesthetizing the digits. These include the traditional four-sided "ring block," the three-sided digital block, the finger web space block, the transthecal block, and the subcutaneous block Morrison (1993),Hill et al. (1995)). It is seen that our participants often prefer the traditional three-sided digital block application. Although technical selection does not have a clear advantage over each other in the literature, the mechanical pressure effects of injecting a solution into a potentially closed area is a situation that should always be kept in mind, especially in blocks at the base of the finger. In cases where circulation is impaired such as fractures, dislocations, crush injuries, it is thought that the application of 4-sided and 3-sided local anesthesia may adversely affect the circulation with mechanical effect and alternative methods should be used. A few small randomized studies comparing transthecal blocks with traditional digital blocks, which were not favored by our survey respondents, found them to be equally effective with similar onset and duration of anesthesia, although in some studies the transthecal technique was slightly more painful and technically more challenging Keramidas et al. (2004). The authors of a small observational study suggests that transthecal block works through subcutaneous administration of anesthetic Sonohata et al. (2009). Although this is unlikely, there is a theoretical risk of flexor tendon injury from the transthecal approach. According to one case series, the technique is effective in children Antevy et al. (2010). A few small randomized studies comparing subcutaneous blocks with both transthecal and conventional blocks have found the subcutaneous approach to be equally effective and less painful in some situations Cannon et al. (2010),Okur et al. (2017). With this result, we think that the traditional teachings in the clinics are more effective than the literature and current sources in the application form and dose of the people. The choice of anesthesia needs to be adjusted according to the length of analgesia desired. In our survey, the most frequently used factor independent of time was asked, and lidocaine had the highest usage rate. We think that it has the highest preference in clinics due to its easy availability and traditional use. When we questioned the use of epinephrine with local anesthesia, the majority of the participants stated that they did not use epinephrine. In the literature, epinephrine causes local vasoconstriction, reduces bleeding and allows anesthesia to stay in tissues for a longer time. However, the digital arteries pass near the digital nerves and injecting epinephrine at the base of the finger causes vasoconstriction of these vessels Altınyazar et al. (2004), which may increase the risk of digital ischemia in susceptible individuals. Because of the risk of vasoconstriction leading to distal necrosis, digital blocks are taught to be performed without epinephrine. However, recent studies provide no evidence of this event Silva et al. (2020),Mantilla-Rivas et al. (2019)). Although there is no clear evidence of ischemia in recent studies, the use of epinephrine, which has a vasoconstrictive effect, to reduce bleeding or increase the duration of anesthesia is not considered necessary by our participants, similar to the literature.
Although data on efficacy are somewhat limited, a number of measures have been proposed to reduce anesthetic pain Zilinsky et al. (2005). These include: buffering the solution with sodium bicarbonate Bartfield et al. (1993),Cornelius et al. (1996)), using small needles (27 or 30 gauge), slow injection subcutaneous rather than intracutaneous injection warming the anesthetic to body temperature Waldbillig et al. (1995). The clinical literature remains unclear as to whether adding sodium bicarbonate to lidocaine plain or lidocaine with epinephrine improves the quality of peripheral nerve block. In addition, the effect of bicarbonate on the onset of action of lidocaine in peripheral nerve block is controversial. For example, chow et al. Chow et al. (1998) found that adding 8.4% sodium bicarbonate to epinephrine (1:200,000) and 1.5% lidocaine hydrochloride (1:10) did not accelerate the onset of analgesia in axillary brachial plexus block. However, adding sodium bicarbonate at the same concentration and volume ratio to 2% lidocaine with and without epinephrine (1:100,000) shortened the onset of peribulbar anesthesia (20). Apart from its effects on baseline, the effects of bicarbonate on the depth and duration of peripheral nerve block with lidocaine has not been previously described. It was considered as a method that the participants did not prefer during local anesthesia in our survey of anesthesia, whose pain reduction and buffering effect are known in the clinical literature and the effect on the depth of which is unknown.
It was seen that the answers received in the question of the dose amount used in digital block applications were different from the maximum application doses in the literature, and the general approach was that the applied dose was kept at lower levels. It has been seen that the studies on dose related to the dose in the literature or the internet, where the participants continue to learn about the dose from their senior doctor friend, are not at sufficient levels. The percentage of local anesthetics in the ampoule and the active ingredient in the market should be known for the most appropriate anesthesia and attention should be paid to the maximum doses shown in Table 1.
When we questioned whether there was a change in the amount of dose administered in cases such as Diabetes Mellitus, chronic renal failure, and peripheral vascular disease, our aim was to evaluate whether additional disease was questioned before the application, whether these diseases had an effect on the local and systemic effects of the anesthetic agent, and whether the dose to be administered changed. LAST syndrome is the most feared complication when the local anesthetic substance enters the systemic circulation, apart from its local effects. LAST is not encountered very often due to its low level of digital block and low subcutaneous absorption. However, it is useful to know some situations related to the general use of local anesthetics. older patients have consistently been shown to be at greatest risk of LAST Gitman & Barrington (2018). Due to low plasma concentrations of binding protein in neonates and infants, it is recommended to reduce the dose by 15%, especially in children younger than 4 months. Patients with severe kidney disease not only have a reduced hyperdynamic circulation and clearance of LA 's, but also have an increased concentration of α1-acid glycoprotein. As a result, free plasma concentrations are largely unchanged, and dose reduction is usually unnecessary unless the patient is uremic with metabolic acidosis Pere et la. ,Pere et al. (2003)). Again, isolated hepatic dysfunction does not require dose adjustment for single-dose regional anesthesia techniques, despite decreased hepatic clearance of LAs. Patients with severe cardiac dysfunction is particularly susceptible to LA-induced myocardial depression and arrhythmias due to hepatic and renal perfusion leading to decreased metabolism and elimination, respectively. Dose reduction is unnecessary in mild to moderate heart failure where tissue perfusion is maintained, but is recommended in severe heart failure Rosenberg et al. In general, the presence of additional disease is not affected by systemic diseases due to the low subcutaneous systemic absorption of the local anesthetic agent and the inability to inject at high levels for digital block, but in some cases, it should be used with caution and dose reduction may be necessary. When the local effects are evaluated, considering that dangerous circulation is seen in the case of peripheral vascular disease and that mechanical effects may adversely affect the circulation in digital block application, dose reduction or alternative application selection should be considered. The selection, dose and type of anesthesia should be carefully selected by evaluating the distal circulatory disorder, tendency to infection and neuropathic involvement due to diabetes mellitus complications
In the question we asked about dose adjustment in obese patients, the participants generally stated that dose adjustment is not necessary. The optimal dose scale in obese patients is not clear in the use of local anesthetics. There are not enough studies in the literature on the application of digital block in obese patients. In the studies performed, it was stated that the local effect was sufficient on brachial plexus block or sciatic nerve block in obese patients, and it was stated that the results were good regardless of the body mass index, but information about the applied dose was not included.
In the two questions we asked the participants, our aim was to question whether the dose given for each finger and the dose used in the lower or upper extremities changed. According to the answers we received from our participants, the majority thought that the method and dose did not change for the fingers and toes and for any finger to be anesthetized. In the literature, the application method and the application dose are specified as standard and clearly, but the amount of dose that can be used on the fingers or toes or any finger is not specified separately.
Our participants were asked multiple choice about the complications they encountered. The answers were similar to the clinical literature.
5. Conclusion
Of course, the value of personal experiences gained over the years cannot be ignored, but these experiences can be renewed under any circumstances and preferences based on experience should be compatible with scientific facts. Our study was to investigate the compatibility of digital block applications with current literature for specialists and residents working in the fields of Emergency medicine, Orthopedics and Traumatology, Plastic and Reconstructive surgery and Anesthesia and Reanimation, and to reveal the misconceptions in digital block application. Therefore, the results of this survey cannot be used as a recommended guideline. However, the results of this survey are cautionary for the need to review digital block administration and, in particular, the optimal dose selection. We believe that it is necessary to improve the level of knowledge about the secure digital block application, which we frequently encounter in clinics and which we have to use in our daily routine, to increase awareness on this issue and to take necessary precautions. For patient safety, it is necessary to prevent complications related to digital block applications, to specify contraindications, to know the properties of the anesthetic agents that can be used and the doses that can be applied. As a result, information we think we know may not actually be true. For this reason, we think that scientific teachings should replace personal teachings and experience-based practices in the digital block application.
CONFLICT OF INTERESTS
None.
ACKNOWLEDGMENTS
All authors declare that they have no conflict of interest.
Ethical approval
This study received approval from Çanakkale 18 Mart University Faculty of Medicine Ethics Committee.
REFERENCES
Altınyazar, H. C., Ozdemir, H., Koca, R., & Demirci, M. (2004). Epinephrine in Digital Block: Color Doppler Flow Imaging. Dermatologic Surgery, 30(4), 508-511. https://doi.org/10.1097/00042728-200404000-00008
American Academy of Pediatrics, & American Academy of Pediatric Dentistry; Cote, C. J., Wilson, S., & Sedation Working Group. (2006). Guidelines for Monitoring and Management of Pediatric Patients During and After Sedation for Diagnostic and Therapeutic Procedures: An update. Pediatrics, 118(6), 2587-2602. https://doi.org/10.1542/peds.2006-2780
Antevy, P. M., Zuckerbraun, N. S., Saladino, R.
A., & Pitetti, R. D. (2010). Evaluation of a Transthecal Digital
Nerve Block in the Injured Pediatric Patient. Pediatric Emergency Care, 26(3),
177-180. https://doi.org/10.1097/PEC.0b013e3181d1eae1
Bartfield, J. M., Ford, D. T., & Homer, P. J. (1993). Buffered Versus Plain Lidocaine for Digital Nerve Blocks. Annals of Emergency Medicine, 22(2), 216-219. https://doi.org/10.1016/S0196-0644(05)80206-9
Cannon, B., Chan, L., Rowlinson, J. S., &
Little, M. (2010). Digital Anaesthesia: One Injection or two? Emergency
Medicine Journal, 27(7), 533-536. https://doi.org/10.1136/emj.2009.081349
Chow, M. Y. H., Sia, A. T. H., Koay, C. K., &
Chan, Y. W. (1998). Alkalization of Lidocaine Does not Hasten the Onset
of Axillary Brachial Plexus Block. Anesthesia & Analgesia, 86(3), 566-568.
https://doi.org/10.1097/00000539-199803000-00024
Cornelius, P., Kendall, J., Meek, S., & Rajan, R. (1996). Alkalinisation of Lignocaine to Reduce the Pain of Digital Nerve Blockade. Journal of Accident & Emergency Medicine, 13(5), 339-341. https://doi.org/10.1136/emj.13.5.339
Dadure, C., Sola, C., Dalens, B., & Capdevila, X. (2015). Concomitant Anesthesia in Children. In R. D. Miller (Ed.), Miller's Anesthesia (8th ed., 2718). Elsevier.
De Buck, F., Devroe, S., Missant, C., & Van de Velde, M. (2012). Regional Anesthesia Outside the Operating Room: Indications and Techniques. Current Opinion in Anaesthesiology, 25(4), 501-507. https://doi.org/10.1097/ACO.0b013e3283556f58
Gitman, M., & Barrington, M. J. (2018). Local Anesthetic Systemic Toxicity: A Review of Recent Case Reports and Registries. Regional Anesthesia and Pain Medicine, 43(2), 124-130. https://doi.org/10.1097/AAP.0000000000000720
Hill, R. G. Jr., Patterson, J. W., Parker, J. C., & McKay, P. L. (1995). Comparison of Transthecal Digital Block and Traditional Digital Block for Anesthesia of the Finger. Annals of Emergency Medicine, 25(5), 604-607. https://doi.org/10.1016/S0196-0644(95)70171-0
Keramidas, E. G., Rodopoulou, S. G.,
Tsoutsos, D., & Koullias, N. (2004). Comparison of Transthecal
Digital Block and Traditional Digital Block for Anesthesia of the Finger.
Plastic and Reconstructive Surgery, 114(4), 1131-1134.
https://doi.org/10.1097/01.PRS.0000135848.60764.AE
Knoop, K., Trott, A., & Syverud, S. (1994). Comparison of Digital Versus Metacarpal Blocks for Repair of Finger Injuries. Annals of Emergency Medicine, 23(6), 1296-1300. https://doi.org/10.1016/S0196-0644(94)70355-8
Mantilla-Rivas, E., Tan, P., Zajac, J., Tilt,
A., Rogers, G. F., & Oh, A. K. (2019). Is Epinephrine Safe for
Infant Digit Excision? A Retrospective Review of 402 Polydactyly Excisions in
Patients Younger than 6 Months. Plastic and Reconstructive Surgery, 144(1),
126e-133e. https://doi.org/10.1097/PRS.0000000000005774
Morrison, W. G. (1993). Transthecal Digital Block. Archives of Emergency Medicine, 10(1), 35. https://doi.org/10.1136/emj.10.1.35
Okur, O. M., Şener, A., Kavaklı, H. Ş., Genç, S., & Kunt, M. M. (2017). Two Injection Digital Block Versus Single Subcutaneous Palmar Injection Block for Finger Lacerations. European Journal of Trauma and Emergency Surgery, 43(6), 863-868. https://doi.org/10.1007/s00068-016-0695-7
Pere, P. J., Ekstrand, A., Salonen, M., Mäkinen,
K., & Rosenberg, P. H. (2011). Pharmacokinetics of Ropivacaine in
Patients with Chronic Renal Failure. British Journal of Anaesthesia, 106(4),
512-521. https://doi.org/10.1093/bja/aer026
Pere, P., Salonen, M., Jokinen, M., Rosenberg, P. H., Neuvonen, P. J., & Haasio, J. (2003). Pharmacokinetics of Ropivacaine in Uremic and Nonuremic Patients After Axillary Brachial Plexus Block. Anesthesia & Analgesia, 96(2), 563-569. https://doi.org/10.1213/00000539-200302000-00047
Rosenberg, P. H., Veering, B. T., &
Urmey, W. F. (2004). Maximum Recommended doses of Local Anesthetics: A
Multifactorial Concept. Regional Anesthesia and Pain Medicine, 29(6), 564-575
https://doi.org/10.1097/00115550-200411000-00010
Silva Neto, O. B. D., Costa, C. F. P. A., Veloso, F. S., Kassar, S. B., & Sampaio, D. L. (2020). Effects of vasoconstrictor use on Digital Nerve Block: Systematic Review with Meta-Analysis. Revista do Colégio Brasileiro de Cirurgiões, 47, e20202346. https://doi.org/10.1590/0100-6991e-20202346
Sonohata, M., Asami, A., Ogawa, K., Kurimoto, S., & Mawatari, M. (2009). Single Injection Digital Block: Is Transthecal Injection Necessary? Journal of Hand Surgery (European Volume), 34(1), 94-95. https://doi.org/10.1177/1753193408096019
Waldbillig, D. K., Quinn, J. V., Stiell, I. G., & Wells, G. A. (1995). Randomized Double-Blind Controlled trial Comparing Room-Temperature and Heated Lidocaine for Digital Nerve Block. Annals of Emergency Medicine, 26(6), 677-681. https://doi.org/10.1016/S0196-0644(95)70036-6
Zahl, K., Jordan, A., McGroarty, J., Sorensen,
B., & Gotta, A. W. (1991). The Effect of Bicarbonate on Mixtures of
Lidocaine, Bupivacaine and Hyaluronidase with or without Epinephrine.
Ophthalmology, 98(2), 239-242. https://doi.org/10.1016/S0161-6420(91)32311-X
Zilinsky, I., Bar-Meir, E., Zaslansky, R., Winkler, E., & Dannon, P. (2005). Ten Commandments for Minimal Pain During Administration of Local Anesthetics. Journal of Drugs in Dermatology, 4(2), 212-216.
 This work is licensed under a: Creative Commons Attribution 4.0 International License
This work is licensed under a: Creative Commons Attribution 4.0 International License
© Granthaalayah 2014-2025. All Rights Reserved.