SCRUPULOUS REVIEW ON ‘INTEGRATED PROCTOLOGY’
Dwivedi Amarprakash 1![]()
1 Professor, School of Ayurveda, D Y
Patil University, Navi Mumbai, India
|
|
ABSTRACT |
||
|
Background- Proctology involves study of rectum and anal canal. Further, in today’s modernized world, shift duties, stressful life, eating of unhealthy foods makes people more prone to the ano-rectal diseases such as fissure, haemorrhoid, abscess, anal fistula and rectal prolapse etc. Modern medical science has treatment alternatives such as conservative treatment for symptomatic relief along with diet- lifestyle modification, and various surgical interventions etc. with due risk and varied prognosis. In Ayurveda, these common ano rectal problems are termed as gud vikar and Ayurvedic texts suggest fourfold treatment for such as Bheshaj (Medicinal treatment), Kshar karma (Herbal caustic paste), Agnikarma (thermal heat burn) and Shastra karma (Surgery). Method- In this review article, information from modern surgery texts in view of definition, aetiology, patho-physiology, sign and symptoms and available treatment options as per stage of disease and a gist of contemporary texts of Ayurveda related to these gud vikaras such as parikartika, gudarsh, gud vidradhi, bhagandar, nadi vran and guda bramsh have been documented to understand integrated and holistic treatment approach towards various ano rectal problems. Result & Conclusion- The article attempts to simplify proctology and touches maximum
aspects of common ano rectal diseases with an integrated approach. Hence,
this article will certainly prove useful to proctologist and researchers
belonging to field of Modern and Ayurveda, to know about integrated
proctology. |
|||
|
Received 1 April 2021 Accepted 20 May 2021 Published 1 July 2021 Corresponding Author Dwivedi
Amarprakash, amar.dwivedi@dypatil.edu DOI 10.29121/jahim.v1.i1.2021.4 Funding: This research
received no specific grant from any funding agency in the public, commercial,
or not-for-profit sectors. Copyright: © 2022 The
Author(s). This work is licensed under a Creative Commons
Attribution 4.0 International License. With the
license CC-BY, authors retain the copyright, allowing anyone to download,
reuse, re-print, modify, distribute, and/or copy their contribution. The work
must be properly attributed to its author.
|
|||
|
Keywords: Haemorrhoid, Fissure, Fistula, Pilonidal
Sinus, Rectal Prolapse, Gud Vikar |
|||
1. INTRODUCTION
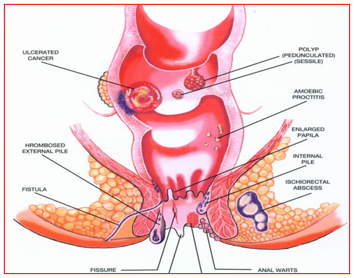
In today’s modernized world, shift duties, stressful life, eating of unhealthy foods makes people more prone to the ano-rectal diseases. The common ano rectal condition includes various skin disease such as allergic rash, fungal infection, dermatitis, eczematous itching etc., skin tags, anal warts, anal papilla, anal polyp, hemorrhoids, anal fissures, abscesses, anal fistula, pilonidal sinus, rectal prolapse and malignancy. Modern medical science has treatment alternatives such as conservative treatment for symptomatic relief along with diet- lifestyle modification, and various surgical interventions etc. with due risk and varied prognosis.
In Ayurveda, these common ano rectal problems are termed as gud vicar. Based on clinical features these conditions can be co related as gudarsh (Haemorrhoids), parikartika (anal fissure), gud vidradhi (abscess), bhagandar (anal fistula), nadi vran (pilonidal sinus) and guda bramsh (rectal prolapse). The Ayurvedic texts suggest fourfold treatment for these gud vikras such as Bheshaj (Medicinal treatment), Kshar karma (Herbal caustic paste), Agni karma (thermal heat burn) and Shastra karma (Surgery).
Further, skin diseases and malignancy is out of purview, and, in this review article we are focusing on ano rectal problems which are commonly seen in proctology practice such as hemorrhoids, anal fissures, abscesses, anal fistula, pilonidal sinus and rectal prolapse pertaining to their diagnosis and management.
In this article aetiology, pathogenesis, clinical manifestation of common ano rectal diseases and various established treatment alternatives from modern surgery and Ayurveda have been dealt in detail. Hence, the article will prove beneficial for surgeons and researchers working in the field of proctology.
Figure 1
|
Figure
1
Various ano rectal conditions |
2. METHODOLOGY
In this review article, information from modern surgery texts in view of definition, aetiology, patho-physiology, sign and symptoms and available treatment options as per stage of disease and a gist of contemporary texts of Ayurveda related to these gud vikaras such as parikartika, gudarsh, gud vidradhi, bhagandar, nadi vran and guda bramsh have been documented to understand integrated and holistic treatment approach towards various ano rectal problems.
This article will certainly prove useful to proctologist and researchers belonging to field of Modern and Ayurveda, to know about integrated proctology.
1) Basic surgical anatomy related to proctology
Proctology involves study of rectum and anal canal. It is important to review basic surgical anatomy related to proctology.
· Rectum - It is the most distal part of gastrointestinal tract. It´s length is nearly14-16 cm.it has proximal end which is located at or just below the level of the sacral promontory. Distal end of rectum is situated at the junction with the anal canal. Rectum covers area of the posterior pelvis as well as the concavity of the sacral bone.
· Anal canal - It is 3 to 4 cm long .it is directed downward and backward from the rectum to end at the anal orifice. It is located within anal triangle of perineum. Its final part of gastrointestinal track. Anal canal is lies completely extra-peritoneal. It is divided into three zone, columnar, intermediate, and cutaneous, respectively.
· Dentate line – It divides the anal canal, above which it is generally insensitive and is lined by columnar epithelium, below which it is highly sensitive (because of somatic innervations) and lined by modified squamous epithelium.
· Sphincter Complex- The sphincter muscle complex is consisting of overlapping of two muscular tubes called as external anal sphincter (EAS) and internal anal sphincter (IAS). The external anal sphincter is derived from striated (skeletal) muscle. It is longer and thicker in nature. The internal anal sphincter is thinner and slightly shorter than external anal sphincter. The intersphincteric groove formed due to difference in length between the two sphincter tubes. Intersphincteric groove is important landmark because of its easily palpated. This intersphincteric space is does not contain any relevant vasculature, so it is potential space of used in surgical dissection
· Blood supply- area of anal canal above pectinate line got blood supply from terminal branch of superior rectal artery (SRA). Superior rectal artery (SRA) is terminal branch of mesenteric artery. The superior rectal vein drains the rectum and upper anal canal, The middle rectal veins drain the lower rectum, and the inferior rectal veins drain the lower anal canal.
· Nerve supply- The pudendal nerve is originating from the fibres of the sacral plexus. It is the main nerve of the perineum.
· Haemorrhoidal plexus- The internal hemorrhoidal plexus lies in the submucosa of the anal canal while External hemorrhoidal plexus lies under the skin of the anal canal. Anatomically location of internal hemorrhoidal plexus located above the dentate line, while External hemorrhoidal plexus located below the dentate line
3. HAEMORRHOID
3.1. DEFINITION
Haemorrhoids, also called piles are masses or clumps of tissues which consist of muscle and elastic fibres with enlarged, bulging blood vessels and surrounding supporting tissues present in the anal canal of an individual. It is a condition characterized by the prolapsed of an anal cushion that may result in bleeding and pain. Dadelszen (2019)
3.2. PATHOGENESIS
The development of haemorrhoidal disease begins from dilatation within the cavernous bodies of the anal cushions primarily due to passing hard stool or straining at defecation, leading to, bruising of engorged venous cushions and rupture of artero-venous shunts resulting in bleeding (spontaneous or during defecation).
3.3. ETIOLOGY
The common etiological factors seen are- Congenital (by birth due to genetic defect), Anatomical (due to no firm support to GI track in pelvic floor), Sedentary lifestyle (Causing over filling of blood vessels), Alcohol (causing hepatitis leading to portal hypertension), Constipation, enlargement of Prostate, Asthma, strenuous work such as weightlifting (causing increase in intra-abdominal pressure and over filling of blood vessels). Similarly, few distinct factors responsible in females are pregnancy, labour phase and uterine fibroids causing increase in intra-abdominal pressure etc.
3.4. CLASSIFICATION
anatomically, haemorrhoids are classified into two types, internal and external respectively. This classification done from location of dentate line. Haemorrhoids located above the dentate line called as internal Haemorrhoid. Haemorrhoid located below the dentate line called as external Haemorrhoid. Internal hemorrhoids are classified into four degrees.
First degree hemorrhoids do not prolapse but comes out from anal canal and cause bleeding. Second degree hemorrhoids prolapse but it self-reduces back into the canal. Third degree hemorrhoids prolapse and need to reduce manually, fourth degree hemorrhoids are irreducible. While we do physical examination, hemorrhoids are typically located in the right anterior, right posterior, or left lateral position (3, 7, and 11 o’ clock position).
3.5. CLINICAL MANIFESTATIONS
3.5.1. EXTERNAL HEMORRHOIDS
Patients usually present with Peri-anal hematoma due to severe straining and per rectum bleeding due to rupture of dilated artero-venous shunts (anal cushion). It has sudden onset of painful lump or swelling at the anus, bluish in colour, covered with smooth shining skin, secondary thrombosis.
3.5.2. INTERNAL HEMORRHOIDS
They are located above dentate line. Bleeding in internal Hemorrhoids is spontaneous and painless.
Acute hemorrhoidal prolapse give excess tender, due to pressure it can create ulceration, and sometime infection too.
3.6. TREATMENT ALTERNATIVES
3.6.1. EXTERNAL HEMORRHOIDS MANAGEMENT
In Acute stage (if patient comes within 48 hrs) with symptoms like severe pain with haematoma, then Analgesics, Anti-inflammatory drugs are prescribed internally along with Xylocaine ointment for local application and hot water Seitz bath with KMNO4 is also advised. Similarly, Laxatives and Antibiotics can be prescribed adjuvantly. Further, if haematoma do not resolve, then it is incised under local anesthesia & the wound is allowed to heal by granulation tissue. If untreated, the haematoma undergoes either resolution or ulceration/suppuration to form an abscess/fibrosis which give rise to skin tag.
3.6.2. INTERNAL HEMORRHOIDS MANAGEMENT
Treatment for internal hemorrhoids decided on the severity of symptoms occurs due to Internal Hemorrhoids. Conservative management done for Internal Hemorrhoids Management
Moreover, various treatment alternatives practiced can be categorized as below-
3.6.3. SCLEROTHERAPY
Sclerotherapy is a procedure used to treat blood vessel malformation. It is also used in Hemorrhoids Management. In Sclerotherapy medicine are injected at the base of the haemorrhoid (into ano-rectal submucosa) above the dentate line. Polidocanol, quinine, urea are some Sclerosing agents. Sclerosing agents shrink the hemorrthiod. Sclerotherapy is effective in first- and second-degree internal haemorrhoids but it is not as effective on large prolapsing hemorrhoids. Sloughing of the mucosa, reaction to the injection, and secondary infections are some rare complications of Sclerotherapy.
3.6.4. BARRON’S RUBBER BAND LIGATION
In this procedure, rubber ring ligature applied to the mucosal covered part of the internal pile through a proctoscope with the help of Barron’s pile gun. It is effective in first- and second-degree internal haemorrhoids but less effective with third degree haemorrhoids. We can think this procedure to alternative to surgery. Macrae and Macleod (1995) Bleeding, secondary infection, and pain is some Common complications of Barron’s Rubber Band Ligation
3.6.5. DOPPLER GUIDED HEMORRHOID ARTERY LIGATION (DGHAL)
Modified proctoscope and Doppler probe used in this method. Modified proctoscope helps to identify the hemorrhoidal arteries. Sutures are placed into the areas of Hemorrhoid arterial. This helps to reducing prolapse.[3] Infection and haemorrhage are Complication of DGHAL. Recurrence rates of this method is only 1%.
3.6.6. INFRA-RED COAGULATION
In this method we transmit infrared radiation on Hemorrhoid. This infrared radiation coagulates the mucosa. It is applied to the apex of each hemorrhoid at top of anal canal, which coagulates tissue protein and dehydrates the cell. It causes actual burn up to the sub-mucosa, causes tissue destruction & evokes inflammatory reaction, ultimately results in scarring. If Infra-Red Coagulation done properly than it will be painless, and we can minimize its complications too.
3.6.7. HAEMORRHOID LASER PROCEDURE
In this, Haemorrhoidal arterial flow feeding the haemorrhoidal plexus is stopped by means of doppler-guided Laser coagulation. It is very popular treatment amongst patients but in practically, Laser photocoagulation does not have any advantage over other treatment modalities. Haemorrhoid Laser Procedure is expensive as well as it has a greater risk of complications like unrecognized deep tissue destruction. Sohn et al. (2001), Endres and Steinhagen (1994)
3.6.8. HAEMORRHOIDECTOMY
Surgical haemorrhoidectomy is practiced in two ways - open and closed haemorrhoidectomy. In open haemorrhoidectomy, pile pedicle is transfixed and excised leaving raw wound surface, whereas in closed haemorrhoidectomy after excision of the pile mass, the wound surface is closed with the help of mucosal flap. Further, for better outcome, lateral sphincterotomy is practiced after surgical haemorrhoidectomy to relieve discomfort and post-operative fissure formation. Mazier (1994)
Haemorrhoidectomy is used in grade III and IV haemorrhoids. It is also used in case of grade I and II haemorrhoids which failed in conservative treatment. The common complications include bleeding, urinary retention, and abscess or fistula (less than 0.01%), whereas rare complications include sphincter damage, anal stenosis (less than 1%) and loss of sensitivity.
3.6.9. STAPLED HEMORRHOIDOPEXY
This is also known as Stapled Anupexis (Longo technique) or MIPH i.e., minimally invassive procedure for hemorroids. It is useful in Grade III and Grade IV haemorrhoids where with mucosal prolapse occurs. In this treatment surgeon take string suture into the mucosa with help of circular stapling device. Location of suture is 2 cm above the superior aspect of the hemorrhoids. Due to this method mucosectomy performed which reduces the prolapsed anal mucosa. It is also disrupting the vascular supply to the hemorrhoids. Hard et al. (2005), Gravié et al. (2005)
3.7. AYURVEDIC PERSPECTIVE
3.7.1. DEFINITION
Hemorrhoids can be co -related with Arsha or Gudarsh mentioned in Ayurvedic texts. Further, Arsha is included in Ashta-mahagada category (amongst 8 diseases which are difficult to treat). Arsha is defined as a disease which produces extreme discomfort to the patient resembling one’s enemy, leading to painful defecation and pile mass formation.
3.7.2. PATHOGENESIS (SAMPRAPTI)
If a non- self-possessed person continuously practices un salutary lifestyle and food habits, particularly indulge in strenuous work-exercise, deliberately holding natural urges or consume incompatible meals, which leads to vitiation of Vata dosh and derangement of digestive fire (jattharagni). This vitiated Vata, further vitiates blood and muscle tissue (Rakta, Maans dhatu) and local blood vessels (pradhan dhamani), travels downwards, and affect sphincters and surrounding anatomical structures in the anal canal, leading to pile mass formation i.e., hemorrhoids (Gud Arsha). Sharma (2010)
3.7.3. TYPES (ARSHA PRAKAR)
Sushrut has described 6 types of Gud Arsha such as – Vataj, Pittaj, Kaphaj, Sannipataj, Raktaj and Sahaj (Congenital). Further, as per clinical manifestation, Arsha is classified into Shushkarsha (Dry or non-bleeding hemorrhoids) and Raktarsha (Bleeding hemorrhoids). 2.7.4 Ayurvedic Management of Arsha Sharma (2010)
Sushruta has advocated fourfold therapy for Arsha such as –
3.7.3.1. BHESHAJA/AUSHADHI CHIKITSA (MEDICINAL TREATMENT)
Bheshaja chikitsa is advocated when symptoms are mild & less complicated with onset less than 1 year & with less vitiated Doshas. The basic conservative Ayurvedic management is primarily aimed at Agni Deepan- Pachan (improving digestion), Vata Anuloman (pacifying bowel movements), Rakta shodhan (blood purifier) – stambhan Chikitsa (Hemostatic medicines) and Mal- Sarak Chikitsa (Laxatives).
The line of treatment can be prescribed as below-
Internal Medicines for Dry Piles - (Shushka Arsha)
1) Kankayan Guti + Triphala Guggulu + Arogyavardhini vati – Each 2 Tab. 3 times a day with lukewarm water after meals.
2) Abhayarishtha - 4 tablespoon with equal amount of water 2 times after meals.
3) Amrutbhallatak Awleha - 1 tablespoon each morning with lukewarm water.
4) Gandharva Haritaki Churna - 1 tablespoon at bedtime with warm water.
Local application in Dry Piles – (Shushka Arsha)
Arshoghn Lep- (Topical Application to promote fibrosis and delay the protrusion)
Such as Snuhi Latex+Haridra, Haridra+Pippali+Gomutra, Nimbadi Malhar etc.
Apply Sarjarasa malhar or Shatadhaut ghruta locally (anal canal)
Fumigate with Guggulu, Vacha, Dhoopa, Ajmoda etc. (Sthanik Dhupan)
Apply Chukra, Kashisadi or Pippalyadi Tail and advice Seitz bath.
Internal medicines for Bleeding Piles- (Rakta Arsha)
1) Praval pishti + Kamaduha ras+ Bolbaddha ras - 2 Tab. 3 times a day with water before meals (given when Pitta dosha is aggravated leading to bleeding piles).
2) Kutajarishta+ Ashokarishta - 30ml each with equal amount of water, twice after meals (if Piles due to IBS).
3) Nagkeshar +Lodhra Churna – 500mg each with butter & warm water 3 times a day.
4) If severe weakness due to bleeding – Mauktik Bhasma 50 mg + Nagkeshar churna 500 mg + Tapyadi loha vati 2-tab BD –with Lohasav 40ml mixed with equal quantity of water twice a day (as hemostatic and to improve haemoglobin due to blood loss).
3.7.3.2. KSHAR KARMA (APPLICATION OF ALKALINE PASTE)
Kshar karma i.e., application of ‘Pratisaraneeya Kshar’ (alkaline-caustic paste) on the pile pedicle is mentioned in Sushrut samhita. This is indicated in Grade II / III non- bleeding internal haemorrhoids where pedicle is Mridu (soft), Prasrut (Extenssive), Avagaadh (Deep seated-internal?) & Uchhrita (Projecting).
The Kshar paste is applied to the dilated pile pedicles with the help of probe under the guidance of specially designed ‘Arsho Darshan Yantra’ resembling slit- proctoscope.
After application, the pile pedicle is washed with Dhanyaamla (sour gruel which neutralises the chemical reaction) and followed by local application of Yashtimadu Ghrita. It is hypothesized that, Kshar karma causes protein coagulation and necrosis of the tissues which slough outs the pile mass. Some Ayurvedic surgeons prepare a distinct Kshar sutra which is mild in nature (Coated only with Snuhi latex + Haridra powder, without use of Kshar) and having fewer coatings as well, for the ligation of pile pedicle. Moreover, this Kshar sutra is different than conventional Apamarg Kshar sutra used in Bhagandar (fistuala-in ano) management.
3.7.3.3. AGNI KARMA (HEAT BURN THERAPY)
This is indicated when pile pedicle is Karkash (Rough), Sthir (Firm), Prithu (Thick) & Kat thin (Hard- fibrosed). Though, there are only anecdotal reports available on role and use of conventional Agni karma in Arsha chikitsa, however, we can definitely co-relate this with IRC, Electro-coagulation and advanced Laser Techniques used for Grade II & III hemorrhoid ablation, in which various heat sources are used to perform thermal/ heat burn. Similarly, Excision of external sentinel tags with the help of thermal cauterization seen in chronic fissure can also be considered as Agni karma chikitsa.
3.7.3.4. SHALYA KARMA (EXCISION OF PILE MASS)
Shalya karma i.e., excision of piles is indicated when pile mass is of Tanu Mool (Narrow Base), Uchhrita (Projecting/Prolapsed) & Kled yukta (Discharging/Bleeding) resembling III grade & IV prolapsed hemorrhoids.
Shalya karma or Arsha Chhedan karma is very much similar to conventional surgical haemorrhoidectomy, in which firstly, each pile pedicle is ligated /transfixed separately with the help of thread followed by excision of pile mass (prolapsed anal cushion). The procedure leaves discomfort and pain at operative site due a raw wound left after excision, which heals in due course of time. In spite of all the advancement in the field of surgery, conventional haemorrhoidectomy is believed to be the gold standard of hemorrhoid treatment, due to safe, cost effective and less recurrence rate.
4. FISSURE IN ANO
4.1. DEFINITION
Anal fissure is defined as longitudinal ulcer in the lower end of anal canal; initially appear as an acute tear in the mucosal lining of the anal canal below the dentate line. Williams (2004)
4.2. PREVALENCE & MANIFESTATION OF FISSURE IN ANO
On anal examination it is seen that, posterior midline is most common location of fissure in Ano. However, in females is found that anterior 60% & 40% at posterior site. Reason of this ration is pregnancy of female. During pregnancy tear of perineum occurs which resulting in loose support to the anterior anus Sivalingam (2010)
4.3. TYPES OF FISSURES IN ANO
1) Primary - fissure is situated at midline of anus, mostly having traumatic etiology.
2) Secondary - situated other than midline of anus, and seen in secondary diseases like ulcerative colitis, Crohn’s disease, malignancy, syphilis, diabetes mellitus & trauma.
4.4. CLINICAL FEATURES OF FISSURE IN ANO
1) Pain - Remain after defecation constant up to 2-4 hours (burning or cutting in nature)
2) Hard stool – stony hard or pellet like stool.
3) Sentinel piles - present in chronic fissure in ano.
4) Bleeding - Bleeding is streak like on stool matter on a toilet paper.
5) Abscess – may be due to infection and injury to anal gland.
6) Itching - perianal area remains wet due to continuous discharge from ulcer which results in irritation or itching in perianal region.
On Inspection of Anal region - fissure is visible in midline.
P/R Digital examination – is difficult in acute condition, due to pain and proctoscopy is strictly contra- indicated in such painful condition. Patient may go in shock if done forcefully.
However, in chronic condition - fissure is palpable & tenderness & spasm of sphincter can be noted. Hypertrophic anal papillae are associated with chronic anal fissures which is seen internally at the dentate line. It is a sentinel tag or pile. Fibbers of the internal sphincter may be exposed at the base of the ulcer. On examination it is friable.
4.5. TREATMENT OF FISSURE IN ANO
4.5.1. CONSERVATIVE MANAGEMENT
The aim of treatment of anal fissures is relaxing anal hyper-tonicity and give relief from trauma. Dietary with rich in fibre helps to improve symptoms of fissure in ano. In excess pain and burning sensation, local anesthetic ointment used example 5% lignocaine. Similarly, NSAIDs (with enzymes such as Serrati peptidase or Chymotrypsin) and Antibiotics (preferably Metronidazole or ornidazole combination). Sometimes, if pain is unbearable and not relieved with conservative treatment, inferior haemorrhoidal nerve block can be tried for relief of pain.
To relax hypertonic sphincter tone, we adviced sitz bath. Potassium paramagnet or salt, harridan are some materials used for sitz bath. it is given relief in perineal pain.
Topical application of
In some cases, we give glyceral trinitrate 0.2% ointment (nitric oxide donor) for local application. Its increase anoderm blood flow & relax sphincter tone. With use of this ointment 60% of patients got relief in healing fissures. Headache and orthostatic hypotension are side effect of this treatment.
Botulinum toxin also used to relax anal resting pressures. We advised this treatment in chronic anal ulcers which is not responding to conservative treatment. , 86–100% patients get good response with botulinum injection. There is No adverse effects seen in this tretment.
4.5.2. SURGICAL MANAGEMENT
4.5.2.1. LORD’S ANAL DILATATION
In this management under an anesthesia, Manual dilation and relaxation of the anal sphincter done. Extent of traumatic rupture of the internal sphincter muscles is probable adverse effect of this treatment.
4.5.2.2. SPHINCERECTOMY
In case of high anal sphincter tone and chronic anal fissure sphincterotomy is one of the best treatments. This surgery done by giving local anesthesia, the internal sphincter is divided from the dentate line to its distal most margin at either lateral position. An open or closed technique used for that.
4.5.2.3. FISSURECTOMY
This involves excision of the damaged skin from around anal fissure, along with any ‘sentinel’ skin tags. A triangular incision (v shaped) is made with a surgical knife, starting from anal margin on each site of the fissure. After removal of fibrous band from ulcer bed, edges of fissure sutured with 2-0 chromic catgut with interrupted suture. Usually, fistulectomy is combined with lateral sphincterotomy or Botulinum injection. Recurrence rates of fistulectomy is less than 5%. Incontinence of flatus and soiling and anal stricture are temporary Complications of this treatment.
4.6. AYURVEDIC PERSPECTIVE
The symptom of fissure resembles with parikartika mentioned in Ayurvedic classics. Sushruta has described condition named- parikartika, having ulcerative lesion in the anal canal (due to traumatic origin- bastinetra vyapad) with clinical features such as cutting or burning pain in perianal region extending up to pelvic and groin. Further, Sushruta has mentioned parikartika -as one of the prodromal features of hemorrhoids (purvarup of Arsha). Shastri (2002)
Based on clinical features, parikartika is categorised as – Vataja and Pittaja types, wherein; Vataja has cutting -throbbing pain (vitiation of Vata Dosha i.e Vata prakop due to ruksha, khara, sukshma gun) and Pittaja type has severe burning sensation (vitiation of Pitta Dosha i.e., Pitta prakop due to Ushna, Tikshna gun). The pathogenesis further consists of Rasa Kshay, Rakta dushti, Mansa Kshay and Mala – Purisha dushti. Tewari (2018)
4.6.1. AYURVEDIC MANAGEMENT OF ANAL FISSURE
The treatment involves improving Agni (Agni deepen), relieving Pain, and burning sensation by pacifying vitiated Doshas (Vata-Pitta), correction of constipation (Anuloman, Mal-nihsaran) and promoting wound healing (Vran roman).
In Vataja Type-
1) Tab Triphala Guggulu + Tab Kaishor Guggulu – 2 tab each BD
2) Mauktik bhasma 30 mg + Avipattikar churna 3 gm HS
3) Suranpindi or Haritaki Tikadi - 3Gm – 2 tabs at Bedtime with Luke-warm water
In Pittaja Type-
1) Chandrakala Rasa -2 Tab. 3 times a day.
2) Mauktika Kamadudha - 2 Tab. 3 times a day.
3) Praval pishti vati + Kamdudha – 3 tab each BD
4) Abhayarishtha -30ML with equal amount of water 2 times after meals.
Local Application:
1) Yashtimadhu Ghrit (Topically) / Tail (Matrabasti or Pichu)
2) Shatadhouta Ghrita (Topically)
3) Raktachandan Ghrita (Topically)
4) Hot water -Awagah Svedan in Vataja Type & Chilly water Awagah Svedan (seitz bath) in Pittaja Type. *Triphala quath (decoction) –Awagah Svedan can be advised.
4.6.2. ROLE OF KSHAR IN FISSURE
Role of Kshar in fissure is very limited. In northeast part of the country, some Ayurvedic surgeons apply mild Kshar (Paste) or keep Kshar varti (medicated thread) at the bed of chronic fissure. The mode of action may be, it acts on the ulcer bed and performs lysis of fibrous tissues, or it may stop hyper granulation and promote healing.
Further, some traditional healers are Ligating the External Sentinel tags, present in Chronic Fissure with the Ksharsutra. Further, it has been documented that, ligation of Ksharsutra with the help of Needle/ Ksharsutra probe covering Fissure-bed from posterior aspect by making aitrogenic tract is also practiced, allowing Ksharsutra to cut-through. Moreover, considering the unscientific approach and severity of pain - burning in rough ulcer, the acceptance by patient for the above management is doubtful.
5. ANO-RECTAL ABSCESS
5.1. DEFINITION
An abscess can define as collection of pus within the any tissue of the body. Redness, pain, warmth, swelling are Signs and symptoms of abscesses. Bacterial infection is main cause of abscess. Cryptoglandular epithelium lining the anal canal is first place of stating of an anorectal abscess. The internal anal sphincter is act as a barrier to prevents the infection. This barrier can be breached through the crypts of Morgagni, which can penetrate through the internal sphincter into the intersphincteric space.
5.2. CLASSIFICATION
first infection enters into the intersphincteric space, further infection can involve the intersphincteric space to ischiorectal space, or even the supralevator space. Ano-rectal Abscess can be classified as ischio-rectal abscess, peri-anal abscess, inter-sphincteric abscess and supra-levator abscess.
5.3. ANO-RECTAL ABSCESS MANAGEMENT
Treatment- in most of infections antibiotics is best solution, but here antibiotics alone will not enough to cure an abscess. For best results abscess should be open and drain properly. This procedure is called as incision and drainage (I&D). Sometimes draining can occurs itself by our body.
Incision and Drainage procedure- Cruciate incision is taken, Pus pockets broken and cavity- pus collection is drained followed by roller- guaze dressing (allowing healing from bottom to top) adjuvant to appropriate antibiotic coverage and analgesic drugs. Further, pus is sent for culture& sensitivity (Antibiotics, AFB).
In patients with recurrent anorectal abscess always consider some associated underlying diseases such as Crohn’s, Ulcerative Collitis, Rectal Cancer and Koch’s etc.
5.4. AYURVEDIC PERSPECTIVE
Based on resembling clinical features, we can co relate abscess condition with gud vidradhi. Further, vidradhi is grossly classified into Apakwa Vran-Shoth (un rippen inflamatory-stage and Pakwa vidradhi (rippen abscess stage).
5.5. MANAGEMENT
In Apakwa (un rippen)-stage the treatment includes, avagah swedan (fomentation), vat-patradi lep (medicated paste), and/or raktamokshan (Jalaoka) to resolve Vran-Shoth. In Pakwa (rippen)-stage, daaran, bhedan and or patan karma (I &D) is done followed by dressing with triphala or panchvalkal kwath adjuvant to Triphala Guggulu / Sapta Vinshati Guggulu and Gandhakrasayan vati internally.
6. FISTULA-IN-ANO
6.1. DEFINITION
Fistula-in-Ano is an inflammatory tract lined by unhealthy granulation or fibrous tissues, which has an External opening in the peri anal skin and an Internal opening in the anal canal or rectum. Jadhavji and Acharya (2003)
6.2. ETIOLOGY OF FISTULA
Etiology in modern medical science is divided in two categories.
NON-SPECIFIC- This is due to Crypto glandular infection, Sequel of Anorectal abscess, or Previous Pyogenic Abscess.
SPECIFIC- These are the diseases or underlying pathologies which can result in fistulous condition like Tuberculosis, Anal fissure, Ulcerative colitis, Crohn’s disease, Leukemia, Colloid Carcinoma, Foreign body intrusion, Pelvic inflammation, Trauma, Exposure to radiation, Lymphogranuloma venerum, Immuno compromised state, Infectious dermatitis & other Rectal, Obstetrical or Gynecological operations. Jadhavji and Acharya (2003)
6.3. CLINICAL FEATURES OF FISTULA
The cardinal feature of fistula in ano is recurrent discharging boils with single or multiple external openings.
The other clinical manifestations as per modern science includes granulation tissues pouting out from the external opening of the fistula (chronic cases). Nodule touch felt on ano rectal wall in its internal opening. Similarly, tenderness and indurations of the skin in inflammatory stage with fever may be present due to suppuration.
6.4. CLASSIFICATION OF FISTULA
There are many classifications available in modern text viz. Milligan Morgan & Goligher’s classification, Ernst mile’s classification, Melcheor Goz classification, Steltzner classification and Park’s classification (as per relation with sphincters) however, Milligan Morgan & Goligher’s classification is more practical.
Low level fistula: these types of fistulae open into the anal canal below the ano rectal ring. They are further subdivided into Subcutaneous, Submucosal, Intersphincteric & Suprasphincteric fistula.
High level fistula: High level fistula open into the anal canal at or above the ano- rectal ring. They are further sub divided into Extra sphincteric or Supra levator, Trans sphincteric & Pelvi- rectal fistula. Jadhavji and Acharya (2003)
6.5. MANAGEMENT OF FISTULA IN ANO
Treatment of low-level fistula
Fistulotomy - In fistulotomy, track open with the knife and scrapping of the unhealthy granulation tissues done with the wall of the fistula.
Fistulectomy - In this, track open with the knife and whole track with the fibrous tissue is excised. The cavity is packed with roller gauze. Jadhavji and Acharya (2003)
Treatment of high-level fistula
Supra levator fistula: Supra levator fistula is generally cause secondary to some disease. Crohn's disease, Ulcerative colitis, Carcinoma, foreign body are primary disease which further causes supra levator fistula. In this condition all treat primary condition & the fistula is ignored.
Trans-sphincteric fistula with a perforating secondary track: For Trans-sphincteric fistula with a perforating secondary track the surgery is done in two different methods are in practice.
Method 1- Fistulotomy of lower track with scapping of high fistula.
Method 2 - Gabriel’s two stage operation- In this method, surgery is performed in two stages:
Stage 1 - Fistulotomy of lower track with Seton ligation.
Stage 2 - After 6 weeks, Fistulectomy of remaining track with Seton ligation.
Treatment Alternatives- Apart from conventional surgical intervention, there are few other treatment modalities practiced with varied prognosis. Anal Fistula Plug, Fibrin Glue, VAAFT (Video Assessed Anal Fistula Treatment), LIFT (Ligation of inter sphincteric fistula tract) are some alternatives treatments for that.
Similarly, an Ayurvedic para surgical procedure commonly known as Ksharsutra therapy (Ayurvedic Cutting Seton) is also recommended and successfully practiced in India and sub-continent with comparatively less complications particularly in low anal fistulas.
6.6. AYURVEDIC PERSPECTIVE
6.6.1. DEFINITION OF BHAGANDAR IN SUSHRUT
A disease or condition causing severe referred pain to Bhag (Perineum), Gud (Anal) & Basti (Pelvis) is called Bhagandar. The manifestation begins with a boil (Abscess) around peri anal region and if it is not treated properly can burst & convert into discharging track and is named as– Bhagandar. Shastri (2002)
6.6.2. PATHOGENSIS
Pathogenesis mentioned in Sushrut
Sushrut has beautifully described the pathogenesis of Bhagandar. He quoted that when a person is indulged in Mithya Aahar- Vihaar (un salutary lifestyle & food habits), Vaat in his body get aggravated & localized in anal canal. Further, it vitiates the muscle & blood, giving rise to Pitika (Boil) & if this condition is not treated in time, this Pitika suppurate & burst resulting in a discharging track which is known as ‘Bhagandar.’ Shastri (2002)
Pathogenesis mentioned in Charak samhita
Charak has described pathogenesis of Bhagandar in very practical way. As per Charak etiological factors like Krimi Bhakshan, Asthi Kshanan, Pravahan, Utkataasan & Horse riding vitiate the Doshas & Causes Boil at peri anal region which after Suppuration burst &turns to Bhagandar.
In this context Krimi Bhakshan can be co related with any infection caused by micro-organism or Crypto glandular infection. Trin- Asthi Kshanan can be considered as sought of Bhagandar due to Trauma, Pravahan is straining during act of defecation as seen in Dysentery etc. causing inflammatory changes in rectum and anal canal and Utkataasan is continuously sitting in Squatting posture causing ischemia and micro necrosis at pressure point. Similarly, cause like Horse riding in present scenario can be compared with over motor bike driving causing ischemic necrosis at cellular level triggering inflammation and infection.
6.6.3. CLINICAL FEATURES MENTIONED IN SUSHRUT
The sign and symptoms of Bhagandar are elaborated nicely in Ayurvedic text. Even the prodromal features (Purv roop) has been described, so as to diagnose the condition at the earliest for better management. The pro dromal features of Bhagandar mentioned are pain at anal region after deification, itching and swelling around peri anal region, lower backache with pain at anal region after long driving and suppurative -induration (Abscess formation) at peri anal region associated with pain & burning sensation at anal region. Shastri (2002)
Bhagandar is manifested by severe refereed pain to Bhag (Perineum), Gud (Anal) & Basti (Pelvis). The clinical features are described beautifully as per the stages i.e., progress of disease commonly known as Shatkrikal. Also, the cardinal features are further explained as per the predominance of doshas like in Vataj type the discharge is associated with flatus, feces & pricking pain. Similarly, in Pittaj type there is very foul smelling with burning pain and in Kaphaj type there is sticky discharge with comparatively more itching. Shastri (2002)
6.6.4. CLASSIFICATION OF BHAGANDAR
Acharya Sushrut has mentioned five types of Bhagandar. Depending upon the resemblance in clinical presentation, we can co relate these Ayurvedic classifications with modern types of fistulae in ano as follows:
· Shatponak (Vataj) resembles with fistula having multiple openings.
· Ushtagreev (Pittaj) resembles curved Fistula resembling the ‘the neck of camel’
· Parisraavi (Kaphaj) resembles fistula with big cavity & profuse discharge.
· Shambukavart (Sannipataj) is fistula resembling with ‘horse pedal’ or horseshoe.
· Unmargi (Kshataj) can be treated like fistula caused by trauma.
Further, Sushrut has advocated that Vataj, Pittaj & Kaphaj type of Bhagandar are Kashtsadhya (difficult to treat) whereas, Sannipataj & Aagantuj are Asadhya (non-curable).
6.6.5. TREATMENT OF BHAGANDAR (FISTULA) MENTIONED IN SUSHRUT
Acharya Sushrut has beautifully described stage wise treatment of Bhagandar. He has advocated that in unripen stage, one should follow ‘Apatarpan to Virechan’ measures of ‘Vran chikitsa’ (wound management) and once the Pitika achieves the ripening stage, Snehan, Avagah Swedan (oleation and fomentation) of the peri anal region should be practiced. Further, if the Pitika does not resolve then, exploration of the track (Fistulotomy) should be done with the help of fistula probe. After, fistulotomy, Kshar (medicated caustic paste) should be applied, or Agni Karm (cauterization) should be done in the explored bed of ulcer.
Post operatively, for pain management ‘Yashtimadhu ’or ‘Anu’ tail - Sinchan (irrigation of medicated oils over the ulcerative lesion) & Swedan (Seitz bath) is advised to the patient.
In the chronic and recurrent conditions, where the fistula track is partially fibrosis or the track is not patent, ‘Bhagandar nasahan tail’ (medicated oil) can be irrigated through the fistula track to make the track patent & in those who are not willing to undergo surgery.
Further, in ‘Visarp Nadi Stanrog chikitsa’ chapter Sushrut has described that those patients who are not willing or not fit for surgery, Nadi vran (sinus) can be treated with ‘Ksharsutra.’ Furthermore, in this context Acharya Sushrut has quoted that Bhagandar can also be treated with the same ‘Ksharsutra.’ Shastri (2002)
7. PLIONIDAL SINUS (SHALYAJ NADIVRANA)
7.1. DEFINITION
A ‘Pilo nidal sinus’ is sinus tract which commonly contains hairs. The primary location of this sinus is under the skin in a vertical direction between the buttocks. Mostly it is found above the anus. Young adults and teenagers are more prone to this Conditions. The cases are more in males as compared to females with a ratio of 3:1.
7.2. PATHOGENESIS
Whether it is an acquired or congenital disease is still debatable. The congenital theory for pilonidal sinus was more popular after understanding of the embryological study. It was thought that faulty development of the median raphe in this region leads to dermal inclusion which becomes Pilonidal cyst. According to this theory, these cysts should be lined by cuboidal, and not, squamous epithelium as seen in all cases. The acquired theory is supported by finding the condition occurring in the other parts of the body e.g., between the fingers in barbers, in the axilla, perineum, and on a mid-thigh amputation stump and even in the Umbilicus.
first time this condition found in second world war. Which got very coo moon and named as ‘Jeep Disease’. This cause due to prolong sitting in Jeep vehicles. This predisposes hair ends to be pushed into neighboring hair follicles and to initiate a ‘Foreign body’ reaction. This condition is very painful. Sivalingam (2010)
The origin of Pilonidal disease is not fully known but we assume that Congenital or Hereditary abnormality, Hormones, Hair, Friction, and Infection are condition which led to this disease
7.3. CONSERVATIVE MANAGEMENT
Asymptomatic PNS- Meticulous depilation and local hygiene are advised.
Symptomatic PNS- Antibiotics, Anti-inflammatory, Analgesics, and depilation is advocated in acute abscess.
Phenol injection- This is done under closed technique. Injection of phenol inserted into a sinus under local anesthesia. This injection do sclerosis via gradual closure. Need of time, frequent repetition, high recurrence rate are some drawbacks of this technique.
7.4. SURGICAL MANAGEMENT
The number and variety of techniques are available for treating PNS. Every technique has its own benefit and drawbacks too in short no single procedure is superior in all respects.
Incision and drainage is commonly practiced procedures.
7.5. AYURVEDIC PERSPECTIVE
The disease clinically simulates with Shayla nadi vrana described by Sushruta Samhita. Acharya Sushruta has mentioned a minimally invasive para surgical procedure for Nadi vrana. Endres and Steinhagen (1994) Acharya Sushruta, the father of surgery has given detailed description in detail regarding the Nadi or sinus in the chapter of Visarpa nadi stanaroga nidana (10th chapter of Sushruta Samhita Nidana Sthana). He recommended that if inflammatory swelling is ignored even during these stages of suppuration, then it may result in chronic granulating tract & is termed as Nadi which is like a test tube, the exudates remain in movement therein. Moreover, if such suppurative swellings are neglected and not managed properly by Shalya karma in good time it will be responsible for the persistence of chronic Nadi (sinus).
Besides, Acharya Sushruta has advocated that any retained or hidden foreign body in such a chronic granulating tract of discharging nature will also be responsible for the persistence of (sinus) Nadivranas broadly of two types viz., Doshaj (acquired) and Agantuja (traumatic). Surgical methods generally emphasized as excision of the sinus tracks followed by healing of a wound by primary intention. Shastri (2002)
Modified Ksharsutra technique -
Procedure can be named as- partial sinusectomy adjuvant to Ksharsutra ligation. The step includes excision of External openings under local anesthesia, removal of embedded hair follicles, track cleansing with antiseptic solution, and ‘Ksharsutra’ application covering entire underlying track for simultaneous cutting and healing. Further, ‘Ksharsutra’ changing done at the interval of every 7 days till the entire track cut down and simultaneous healing of ulcerative lesion achieved.
8. PROLAPSE OF RECTUM (GUDA BHRAMSH)
8.1. DEFINITION
Prolapse of mucous membrane or the entire rectum outside the anal verge is called as rectal prolapse. This condition is common in children and elderly patients. goligher and Dutie (2004)
Rectal Prolapse is classified in 2 types - Partial prolapse & complete prolapse
Partials prolapse- Partial prolapse is founded as common type of rectal prolapse. Prolapse occurs only mucosa and sub mucosa of the rectum.
Complete prolapse- procidentia is another name of complete prolapse. The descend levels of complete prolapse is always more than 3.75 mm. it can be 10-15 cm also. All the layers of the Rectum involved in complete prolapse. Weakened levator ani muscle & supporting pelvic tissues are main cause of complete prolapse. Females and male ration of this prolapse is 6:1.
8.2. AETIOLOGY
The common aetiological factors are decreased sacral curvature and decreased anal canal tone in infants, diarrhoea, cough, mall nutrition- in children, reduced ischio-rectal fossa fat, poorly developed pelvis, neurological cause, fibrocystic disease of pancreas, common in multi-para females- (due to repeated birth injuries to perineum damages perineal nerve supply), weakness of supporting tissue and levator ani muscle, atony of the sphincter, intra-abdominal pressure get increased, stricture urethra, weakness of anus muscle.
8.3. EVALUATION OF RECTAL PROLAPSE
The evaluation is done based on clinical manifestation such as descended rectum is red in colour and often painful, as mass per anum, per rectal digital examination reveals lax sphincter, anteriorly, peritoneal sac comes down, as a pouch which may contain small intestine, and on digital pushing, it reduces with gurgling, fecal incontinence due to disruption of anal sphincter, proplapsed rectal mucosal discharge and pain and bleeding per anum.
For examination doctor advice to patient for squeeze and relax their anal sphincter in same time the doctor has their finger in the patient’s anus. Anal Manometry, Defecography, Sigmoidoscopy, Colocystodefecography are the advanced diagnostic investigations available for confirmation of the condition
8.4. RECTAL PROLAPSE MANAGEMENT goligher and Dutie (2004)
In Children / Infants
1) Digital Repositioning- patient is trained for manual reduction of mass.
2) Sub mucosal Injections (5% phenol in Almond oil)- This is a sclerosing agent which causes aseptic inflammation which leads to fibrosis of mucosa, preventing prolapsed.
3) Surgery- The surgical procedure is similar to rectopexy, here Retro- rectal space is entered, followed by suturing of rectum with Sacrum.
In Adults
1) Local treatment- Submucosal Injections
2) Excision of Prolapsed mucosa (if prolapse is unilateral)
3) Endo-luminal stapling Technique (if circumferential)
4) Surgery- Rectopexy (Abdominal / Perineal)
In surgical practice, perineal approach is preferred as there is no risk of damage to Pelvic autonomic nerves. Thiersch’s Operation- and Delorme's operation are most practiced. Williams (2004), Dwivedi et al. (2002)
8.5. AYURVEDIC PERSPECTIVE
8.5.1. DEFINITION
Based on resembling clinical features, rectal prolapse can be co related with Guda bhramsh. Sushruta has explained Guda bhramsh in 13th Chapter of Nidan sthan named Kshudraroga nidan adhyay. According to Sushrut samhita, vitiation of Vata, congenital weakness of guda are causes of Guda bhramsh. Shastri (2002)
8.5.2. SAMPRAPTI (PATHOGENESIS)
The pathology mentioned for Guda bhramsh are Mitthya Aahar –Vihar (un salutary lifestyle and food habits) such as suppression of urge of defecation, constipation and or frequent lose motions, indulging in strenuous work /activity such as weightlifting and emaciated patient having weaker Rakta & Maans dhatu (and Sira-Snayu) i.e., poor musculature etc.
8.5.3. AYURVEDIC MANAGEMENT
Ayurvedic treatment plan aimed to pacify vitiated Doshas, to avoid the causative factors by necessary modification in lifestyle and food habits, strengthening the Dhatus involved, and correcting constipation / dysentery. Further, it is true to admit/say that Ayurvedic regimen is useful in partial prolapse of rectum only; moreover, complete prolapse ultimately requires surgical correction.
Ayurvedic regimen effective in Guda bhramsh- Shastri (2002)
1) In case of Guda bramsh, the protruded part should be fomented and lubricated with sneha (preferably with Gogh Rita). It should then be gently re introduced in the anus followed by Gofana bandh (T-bandaging) with leather belt (having an opening/ hole laying below anus for passage of flatus).
2) Fomentation and oleation of the affected part should be done frequently with oils / Ghee medicated with drugs such as nirgundi, Bala, yashtimadhu, panchvalkal etc.
3) Similarly, Balya – Bruhaniya formulations (strengthening ligaments, sphincter, and muscle tone) such as Kushmand Avaleh, Sarivadi vati, Shatavari, Krauncha paak and Vata pacifying drugs such as Nishoth, Suranpindi vati, Triphala can be prescribed.
4) Further, use of a very distinct formulation named Mooshak siddh tail, a medicated oil prepared by boiling milk, mahapanchmoola & flesh of mouse is mentioned for panabhyang (to be used internally & locally as pichu).
5) Another, effective regimen for Guda bramsh management is Changeri Ghrut, which is prescribed 10-20 Ml. twice a day with warm water or milk for 3 to 6 months.
6) Kshar karma in Guda bhramsh- Kshar karma i.e., local application of ‘Pratisaraneeya Kshar’ (alkaline-caustic paste) is effectively practiced in early stages of Guda bhramsh i.e., partial prolapsed of rectum. The Kshar paste is applied to the mucosa with the help of probe under the guidance of slit- proctoscope. After Kshar application the mucosa is washed with Dhanyaamla (sour gruel which neutralises the chemical reaction) and followed by local application of Yashtimadu Ghrita. Similarly, Kshar tail- matra basti (Enema) or pichu can also be prescribed with varied results. It is hypothesized that, Kshar karma causes protein coagulation and fibrosis of the tissues which hardens the prolapsed mucosa same as seen with sclerosing agents.
9. DISCUSSION
Proctology involves study of rectum and anal canal. Further, in today’s modernized world, shift duties, stressful life, eating of unhealthy foods makes people more prone to the ano-rectal diseases such as fissure, haemorrhoid, abscess, anal fistula and rectal prolapse etc. Modern medical science has treatment alternatives such as conservative treatment for symptomatic relief along with diet- lifestyle modification, and various surgical interventions etc. with due risk and varied prognosis. In Ayurveda, these common ano rectal problems are termed as gud vikar and Ayurvedic texts suggest fourfold treatment for such as Bheshaj (Medicinal treatment), Kshar karma (Herbal caustic paste), Agni karma (thermal heat burn) and Shastra karma (Surgery).
In this review article, information from modern surgery texts in view of definition, aetiology, patho-physiology, sign and symptoms and available treatment options as per stage of disease and a gist of contemporary texts of Ayurveda related to these gud vikaras such as parikartika, gudarsh, gud vidradhi, bhagandar, nadi vran and guda bramsh have been documented to understand integrated and holistic treatment approach towards various ano rectal problems.
The article attempts to simplify proctology and touches maximum aspects of common ano rectal diseases with an integrated approach. Hence, this article will certainly prove useful to proctologist and researchers belonging to field of Modern and Ayurveda, to know about integrated proctology.
REFERENCES
Acharya, V. Y. T. (2005). Sushrut- Sushrut Samhita With Thecommentaries Nibandh Sangraha Of Dalhanacharya And Nyay Chandrika Of Sri Gayada, Edited By Yadavji Trikamjiacharaya, 2nd Edition, Varanasi Chaukhambha Orientalia 2005, Chikitsa Sthan Chapter 17, 168.
Acharya, V. Y. T. (2007). Sushrut- Sushrut Samhita With Thecommentaries Nibandh Sangraha Of Dalhanacharya And Nyay Chandrika Of Sri Gayada, 3rd Edition, Varanasi Chaukhambha Orientalia 2007, Nidansthan Chapter 5, 491.
Dadelszen, P.V. (2019). The Global Library of Women’s Medicine’s Welfare of Women Global Health Programme.
Das. S.(n.d.). Concise Text Book Of Surgery 4th Edition S.Das Chapter No 54 Rectum& Anal Canal Treatment Of Fissure In Ano- 10-84.
Dwivedi, L. Prologued & Edi-Tor. (2002). Sushruta Samhita Of Sushruta, Text With English Translation By Kaviraj Kunjalal Bhishagratna, Vol.2, Ni-Dan Stahan, Chapter 13, Verse 13 :60. Vara-Nasi, India : Chaukhamba Sanskrit Series 107.
Endres, J.C. Steinhagen, R.M. (1994). Lasers In Anorectal Surgery. Surg Clin North Am, 74, 1415.
Gravié, J.F. Lehur, P.A. Huten, N. Et Al. (2005). Stapled Hemorrhoidopexy Versus Milligan-Morgan Hemorrhoidectomy: A Prospective, Randomized, Multicenter Trial With 2-Year Postoperative Follow Up. Ann Surg, 242, 29–35.
Hard, A. Chan, C.L.H. Cohen, C.R.G. (2005). The Surgical Management Of Hemorrhoids - A Review. Dig Surg, 22, 26-33.
Jadhavji, V. Acharya, T. (2003). Sushruta Samhita Of Sushruta With The Nibandh Sangarh Commentary Of Shree Dalhanacharya, Varanasi : Publisher Chaukhambha Subharti Prakashan, Nidanasthana Chapter, 307-308.
Macrae H.M. Macleod R.S. (1995). Comparison Of Hemorrhoidal Treatment Modalities. A Meta-Analysis. Dis Colon Rectum,38,687.
Mazier, W.P. (1994). Hemorrhoids, Fissures And Pruritus Ani. Surg Clin North Am, 74,1277.
Murthy, K.R.S. (2005). Editor (Fifth Edition), English Translation Of Astang San-Grah Of Vagbhata, Chikitsa Sthan, Chapter 10, Verse 2 :4, Varanasi, Chaukhamba Orien-Talia, 378-379.
Randall, G.M. Et Al. (1994). Prospective Randomized Comparative Study Of Bipolar Versus Direct Current Electrocoagulation For Treatment Of Bleeding Internal Hemorrhoids. Gastrointest Endosc, 40, 403.
Russel, R..CG. Norman S. William & Chris-Topher J.K. Bulstrode. (2004). Bailey & Love’sShort Practice Of Surgery, Editors, (24th Edi-Tion), International Students Edition Pub-Lished By Hodder Arnold, London, 12-26.
Sharma, P.V. (2010). English Translation Of Text And Dalhan Commentary (Vol.2) On Sushrut Samhita Of Sushruta, Nidan Sthan, Chapter 2, Verse 4, Varanasi, Chaukhamba Vishwabharati, 19.
Shastri, S.R. (2002). Editor, (16th Edition), Bhaishajya Ratnavali- Vidyotini Parishishta Sahit, Hindi Commentary By Ka-Viraj Ambikadatta Shastri, Chapter 8, Verse 8 :556-561. Varanasi, India : Chaukhamba Sanskrit Sansthan, 205.
Sivalingam, P. (2010). Topics In Colorectal Surgery, Jaypee Brothers, Medical Publishers (P), First Edition, Chapter-12, 102-329.
Sohn N. Aronoff J.S. Cohen, F.S. Weinstein, M.A. (2001). Transanal Hemorrhoidal Dearterialization Is An Alternative To Operative Hemorrhoidectomy. Am J Surg, 182(5), 515-19.
Tewari, P.V. (2018). Kashyapa Samhita- Text With English Translation And Commentary Chapter 13. No -2 Sloka- 1,163.
Goligher, J.Dutie, H. (2004). Horold Nitin Surgeryof Anus, Rectum And Colon, 5th Edition, New Delhi AITBS, Publishers And Distributors, Reprint2004, Chapter 6,180.
Williams, N. (2004). Bailys & Loves Short Practice of Surgery 24th Edition Chapter 72 1253-1254.
 This work is licensed under a: Creative Commons Attribution 4.0 International License
This work is licensed under a: Creative Commons Attribution 4.0 International License
© Granthaalayah 2014-2021. All Rights Reserved.