Ameliorative effect of polyherbal formulation for restoring liver health: A systematic review
Dr. Soumendra Darbar 1![]()
![]() , Dr. Sangita
Agarwal 2
, Dr. Sangita
Agarwal 2![]()
![]() , Dr. Srimoyee Saha 3
, Dr. Srimoyee Saha 3![]()
![]() , Dr. Maitrayee
Banerjee Mukherjee 4
, Dr. Maitrayee
Banerjee Mukherjee 4![]()
![]()
1 Principle Investigator and Scientist, Research and Development Division, Dey’s
Medical Stores (Mfg.) Ltd., 62, Bondel Road, Kolkata-700019, West Bengal, India
2 Associate
Professor, Department of Applied Science, RCC Institute of Information
Technology, Canal South Road, Beliaghata,
Kolkata700015, India
3 Research
Scientist, Faculty Council of Science, Jadavpur University, Kolkata-700032, West
Bengal, India
4 Assistant Professor and Head, Department of Physiology, Krishnagar
Government College, Krishnagar, Nadia, India
|
|
ABSTRACT |
||
|
Herbal
medicines have been used for a wide range of ailments since ancient times.
Two methods are used in Ayurvedic medicine formulation: one involves
employing a single herbal preparation, or multiple combinations of them.
Polyherbal formulation is the term for the later.
Combining different herbs and plants to treat different medical diseases or
to enhance general health is known as polyherbal medicine. Many civilizations
all over the world have been using this kind of traditional medicine for
centuries, and it is still commonly used today. Due to the active
phytoconstituents found in single herbs, which are typically present in
minute amounts and occasionally insufficient to produce the desired
therapeutic effects, multi herb formulations have a well-established track
record. According to scientific research, combining these plants with
different potencies may theoretically result in a greater effect than using
each plant alone or the sum of their individual effects. Positive
interactions between herbs can therefore produce synergistic effect, which may take the form of pharmacokinetic or
pharmacodynamic synergism. The great efficacy of polyherbal formulations in
treating a wide range of illnesses accounts for their popularity. The growing
demand of polyherbal formulations necessitates further scientific
investigation in this area. |
|||
|
Received 24 April 2024 Accepted 21 May 2024 Published 21 June 2024 Corresponding Author Dr. Soumendra Darbar, dr.soumendradarbar@deysmedical.com
DOI 10.29121/jahim.v4.i1.2024.53 Funding: This research
received no specific grant from any funding agency in the public, commercial,
or not-for-profit sectors. Copyright: © 2024 The
Author(s). This work is licensed under a Creative Commons
Attribution 4.0 International License. With the
license CC-BY, authors retain the copyright, allowing anyone to download,
reuse, re-print, modify, distribute, and/or copy their contribution. The work
must be properly attributed to its author.
|
|||
|
Keywords: Ayurveda, Polyherbal Formulation,
Traditional Medical System, Liver Illnesses, Hepatoprotective, Liver Tonic |
|||
1. INTRODUCTION
Raw herbs gave way to synthetic pharmaceuticals in the first part of 19th century when scientists started to extract and alter the key ingredients in herbal remedies. Yet, despite their potent pharmacological action, synthetic medications are shown to be comparatively not only costly but also have multitude of unwanted side effects. Since, herbal medications come from nature and are seen to be safer, hence people are turning back to them these days Polyherb. Parasuraman et al. (2014)
Today
approximately 80% of people in underdeveloped nations still receive their
primary healthcare from traditional medicine, which is primarily based on
various plant species. Approximately 500 plants are known to have therapeutic
properties in ancient literature, and 800 species are employed in traditional
indigenous medical systems. India, a country well-known for its biodiversity,
is home to some 40,000 plant species, 15,000 of which are thought to offer
therapeutic benefits. In India, communities use 7,000–7,500 plants to treat a
range of illnesses Kotmire et al. (2024), Ali & Datusalia
(2024), Singh et al. (2024). Numerous plant species are used in the
many native medical systems, including Ayurveda, Siddha, and Unani, to cure
various illnesses Sane (2002), Farnsworth et al. (1985), Abraham & Paridhavi (2013), Kunwar et al. (2010). Due to consumer demand, the $1.5 billion
annual market for herbal medicines is expanding in available widely. Using
plants or plant material, either raw or processed, to cure disease is known as
traditional herbal medicine, currently very popular throughout the globe Ngo et al. (2014).
Owing to the wide range of secondary metabolites that are functionally significant in medicinal plant species, natural products and their associated structures are major sources of newly developed medications Ingawale et al. (2015). Multi-herbal medicines, the blending of several herbs and plant components together to treat different medical issues or to enhance general health is the need of the hour. Throughout history, numerous nations have employed this kind of traditional medicine, which is still commonly used today. When many herbs are combined in a recipe, the synergistic effect occurs, in which the various components cooperate to maximize the beneficial effects and minimize any possible negative consequences Iroanya et al. (2014). Herbal remedies come in a variety of formats, such as tinctures, pills, and topical preparations. They are frequently tailored to the specific needs and symptoms of the patient Saleem et al. (2020). These formulations have long been utilized to treat liver illnesses throughout cultures, and new research has demonstrated encouraging outcomes in their hepatoprotective properties with few adverse effects.
Liver, which is the largest glandular organ in the body and performs myraid of function to an extent more functions than any other human organ. Liver plays a crucial function in human metabolism; the entirety of a person's blood supply flows through it many times each day Alvari et al. (2012). Liver is responsible for the production and secretion of bile, as well as the production of blood clotting proteins prothrombin and fibrinogen, as well as the mucopolysaccharide sulfuric acid ester heparin, which aids in preventing blood clots in the bloodstream. Sugar is transformed into glycogen by the liver Parveen et al. (2022). Liver illnesses are now one of the leading global causes of morbidity and death in both humans and animals. Liver illnesses, which include cirrhosis, hepatitis, liver failure, and related consequences, represent a significant global public health concern. Since, these conditions have an impact on human health Ali & Kumar (2015), liver protection becomes crucial. Hepatoprotective substances are essential for reducing the harm that chemicals, medications, and poisons can do to the liver. Liver disorders have long been treated with plant medicines in India's traditional medical system Shaik et al. (2012). Combining botanical elements from conventional medicine with herbal formulations offers a viable way to treat liver diseases. Their multi-targeted approach to treating complicated disorders has contributed to their appeal, indicating a shift in emphasis toward these formulations Vargas-Pozada & Muriel (2020). This review focused on the potential and reach of polyherbal medicines both locally and globally, while also emphasizing the significance of Ayurveda and polyherbal formulations (PHF).
2. Benefits of polyherbal formulation over single herb
Plants which are used to make herbal medicines are called botanicals, and each plant has a variety of components which when combined proportionately can produce the required result. The demand for Ayurvedic Darbar et al. (2010), Bhope et al. (2011), Darbar & Chattopadhyay (2010), Benzie & Wachtel-Galor (2011) formulations is rising at a great pace because of growing interest in plant-based formulations. Phytomedicines derived from plants, which vary in species, growing environments, and physiologically active components, are safe and frequently used in combination Spinella (2002).
The
pharmacological substances found in polyherbal formulations are derived from
plants and have the ability to potential to show various effects such as anatgonistic, synergistic, agonistic and potentiative (Figure 1) because of their various active principles
Darbar et al. (2009). Together, these pharmacological principles
result in optimum treatment efficacy and minimal side effects. There are two
ways by which synergism functions, namely pharmacodynamics and
pharmacokinetics, depending on the type of interaction Darbar et al. (2020). When it comes to pharmacokinetic
synergism, the components collectively must help in ADME (absorption,
distribution, metabolism, and elimination). Alternatively, pharmacodynamic
synergism examines the synergistic effect that results from targeting a similar
receptor or physiological system with active ingredients that have similar
therapeutic action. Apart from that, the majority of
times, diseases are thought to be caused by a multitude of factors, which leads
to apparent as well as unforseen symptoms. Here, a blend of herbal remedies may work on
various areas concurrently to offer total relief from the ailment Chorgade (2007), Parasuraman et al. (2014), Sarwar et al. (2011), Karole et al. (2019).
Figure 1

|
Figure 1 Advantages and Therapeutic Applications of Polyherbal Formulation |
The synergistic
effects of polyherbalism provide several advantages
not found in single-herb formulations. Clearly, a single multi-constituent
formulation can have a better therapeutic impact. Because of this, a lower
amount of the natural product would be required to provide the desired pharmacological
action, reducing the potential for negative side effects (Table 1). Furthermore, polyherbal formulations
contain a variety of compounds that combat illness complications; hence,
distinct molecules treat diseases through various mechanisms, offering a
comprehensive therapeutic approach for a given disease state Ramaiah et
al. (2013), Rastogi et al. (2012), Darbar et al. (2018).
Table 1
|
Table 1 Popular Indian Medicinal Plants Used in Herbal Formulation |
||||
|
S. No |
Scientific Name |
Common Name |
Family |
Parts Used in formulation |
|
1 |
Azadirachta indica |
Neem |
Meliaceae |
Leaves |
|
2 |
Andrographis paniculata |
Kalmegh |
Acanthaceae |
Leaves |
|
3 |
Zingiber officinale |
Ginger |
Zingiberaceae |
Root |
|
4 |
Picrorhiza kurroa |
Kutki |
Scrofulariaceae |
leaf, bark, and underground parts |
|
5 |
Terminalia chebula |
Haritaki |
Combretaceae |
Seeds |
|
6 |
Asparagus racemosus |
Shatamull |
Liliaceae |
dried roots |
|
7 |
Eugenia Jambolana |
Jamun |
Myrtaceae |
Fruit & Seeds |
|
8 |
Trigonella graeceium |
Methi |
Fabaceae |
leaves and seeds |
|
9 |
Piper nigrum |
Morich |
Piperaceae |
Seeds |
|
10 |
Ocimum sanctum |
tulsi |
Lamiaceae |
Leaves, Roots, Seeds |
|
11 |
Curcuma longa |
Haldi |
Zingiberaceae |
rhizomes |
|
12 |
Berberis vulgaris |
Barberry |
Berberidaceae |
fruit |
|
13 |
Moringa olifera |
Soanjina |
Moringaceae |
roots, leaves, barks,
seeds, flowers, fruits |
|
14 |
Phyllanthus niruri |
Bhumyamalaki |
Euphorbiaceae |
roots, leaves, fruits |
|
15 |
Solanum nigrum |
Kakamachi |
Solanaceae |
leaves, roots, bark,
and flowers |
3. Limitations of polyherbal formulation
Combining plants
that contain these elements may result in combinations that exhibit more
activity than each extract taken alone. Alternatively, the coexistence of
several components could result in chemical incompatibility, causing
instability Stickel & Schuppan (2007). In India, the majority of Ayurvedic PHFs
are produced and exported, however despite the Drugs and Cosmetic Act's
establishment to regulate production and quality control, the manufacturing of
Ayurvedic herbal preparations is subject to slightly lesser regulations (Table 2). Toxicity studies and clinical trials on
herbal formulations are not required, per good clinical standards, in order for
the maker of Ayurvedic herbal formulations to apply for patents and be granted
manufacturing licenses Girish & Pradhan (2017), Darbar et al. (2000).
Table 2
|
Table 2 Advantages and Disadvantages of Herbal Formulation |
|
|
Advantages |
Disadvantages |
|
Better patients
tolerance as well as acceptance |
Adverse Interactions with
Pharmaceuticals |
|
Safe and effective |
Lack of Regulation |
|
No adverse drug reaction |
Unknown Side-effects |
|
Easily available and found
in large variety and quantity |
Slower Healing than
Pharmaceuticals |
4. Herbal formulation for hepatic dysfunctions
Herbal drugs have become increasingly popular
and their use is widespread. These
polyherbal preparations are marketed as tonics with a variety of purposes,
including growth promoters and appetite stimulants, gastrointestinal and
hepatic regulators, liver tonics and stimulants, and treatments for hepatic
dysfunction and regeneration Darbar et al. (2010). Biologically active chemicals from plants,
such as silymarin, picroliv, ellagic acid, curcumin,
andrographolide, and glycyrrhizin, can be used as appropriate building blocks
for hepatoprotective medications that are both efficacious and targeted Darbar et al. (2020). To obtain the intended antioxidant,
antifibrotic, antiviral, immunomodulatory, and anti-inflammatory effects,
hepatoprotective herbals may also be combined Sharma et al. (2015). These medications will enhance biliary
functions, support hepatic regeneration, and stop liver cell deterioration or
necrosis brought on by narcotics, poisons, and viruses. Additionally, the
bioavailability, stability, and effectiveness of these active compounds may be
enhanced by the use of derivatives Padmanabhan & Jangle (2014), Sivakumar et al. (2014).
5. Mode of action of Polyherbal compounds
Figure 2

|
Figure 2 Liver Detoxifying Pathway by Herbal Formulation |
PHFs have a complex range of hepatoprotective properties that work together to protect hepatocytes against the harmful effects of several hepato-toxins. These mixtures show amazing effectiveness in mitigating harm from substances like CCl4, alcohol, medications, and pollutants found in the environment, enabling the return of healthy liver function Darbar et al. (2021). The presence of several phytoconstituents in herbal preparations is responsible for their antioxidant capabilities. Bioactive constituents likes flavonoids, alkaloids, terpenoids, phenolic acids, and tannins actively play a critical part in reducing free radicals and decrease the load of oxidative stress on hepatocytes. Considering that oxidative stress is a key factor in the development of hepatic pathophysiology, this role is crucial Darbar et al. (2021). These formulations are essential for preventing hepatocyte damage and apoptosis because they suppress lipid peroxidation and reduce ROS (Figure 2). Their anti-inflammatory and antifibrotic qualities are also quite important. Hepatic dysfunction progresses due in part to chronic inflammation and fibrosis Belapurkar et al. (2014). Through modulating proinflammatory cytokines such as IL-1β and TNF-α and blocking key signaling pathways like NF-κB and MAPK, these formulations function as strong anti-inflammatory drugs Hamid et al. (2021). Moreover, they lessen fibrosis by preventing the buildup of extracellular matrix proteins including collagen Rajanna et al. (2021).
The methods by
which these PHFs produce hepatoprotection also heavily involve immunomodulatory
actions Saha & Ghosh (2012), Yadav et al. (2016). Livina, VLS, Clearliv,
BV-7310, Amlycure DS, Livomyn,
PNK, Livergen, Syrup, Livactine,
and Livshis are
among the formulations that contain plants having immunomodulating capacity
like Tinospora cordifolia and Andrographis paniculata, which work together to regulate immune
cell activity and cytokine production. In order to
maintain immunological homeostasis and reduce immune-mediated liver injury,
these benefits fortify immune responses against harm caused by toxins Ghosh et al. (2011), Akbarzadeh et al. (2015).
The hepatoprotective activities of these formulations are mostly attributed to the promotion of cellular activity and liver regeneration. Both the recovery from injury and the restoration of normal hepatic function are guaranteed by the stimulation of hepatocyte proliferation and the manufacture of proteins unique to the liver. Increasing the liver's ability for detoxification is a key component of PHFs' mode of action. By boosting the activity of phase I and phase II detoxification enzymes such cytochrome P450, GSH S-transferase, and uridine diphosphate glucuronosyltransferases, these formulations enhance the liver's capacity to neutralize and remove toxins. Thus, the load on the liver is lessened, reducing the possibility of toxic agent-induced liver damage Pingale et al. (2008). In summary, PHFs have hepatoprotective action because of the intricate interactions between their immunomodulatory, regenerative, antifibrotic, antioxidant, and detoxification-enhancing qualities. As therapeutic approaches, these compositions hold great promise for averting liver injury and preserving general hepatic function.
6. Liver tonic
One of the main organs in the human body is the liver. It aids in both the breakdown of food and the majority of micronutrient absorption Siddiqui et al. (2017), Aladejana (2023). Global concern over chronic liver disease (CLD) is growing. Infection, alcohol misuse, exposure to hepatotoxic medications, autoimmune conditions, and metabolic diseases are among the common etiological factors. Cirrhosis of the liver and its associated consequences are the outcome of the chronic liver disease Kantharia et al. (2023), Gaurav et al. (2023). For this reason, maintaining a healthy liver is essential. Ayurvedic liver tonics is recommended to maintain optimal liver health Khan et al. (2024). However, it has been shown that practically every commercially available liver tonic has antioxidant, antibacterial, and anti-inflammatory qualities Shakya et al. (2022), Abbas et al. (2023). Studies revealed that the well-known liver tonic Liv-52 significantly protected rats' livers against the hepatotoxic effects of carbon tetrachloride (CCl4). Lakshmi et al. (2023), Singh et al. (2023). An ideal replacement for allopathic liver medications is an Ayurvedic liver tonic. Due to their natural qualities, liver tonics (Table 3) can help to maintain healthy liver function and offer quick relief from liver problems.
Table 3
|
Table 3 Popular Polyherbal Liver Tonic in India |
||
|
S. No. |
Popular Liver Tonic in India |
Key Highlights |
|
1 |
LIV 52 |
Protects the liver. |
|
2 |
Dizicure Tonic |
Treats liver and its related issues |
|
3 |
Livray Liver Tonic |
Easily available |
|
4 |
Livncid Ayurvedic Liver Tonic |
Free from side effects. |
|
5 |
Hepano Liver Syrup |
Good for liver health. |
|
6 |
Unilivzyme Syrup |
Promotes fast healing. |
|
7 |
Livray-Ds Ayurvedic Liver Tonic |
Improves liver health. |
|
8 |
Regliv Ayurvedic Liver Tonic |
Improves digestion. |
|
9 |
Hepazyme |
Treats fatty liver. |
|
10 |
Livina |
Hepatoprotective |
With the greatest
Ayurvedic characteristics, India have compiled an exclusive assortment of
herbal syrups (Figure 3). Quality, composition, safety, and
popularity are the factors that determine the ranking of these products.
Figure 3

|
Figure 3 Ten Popular Marketed Liver Tonic |
7. Preference of herbal drugs in modern societies
In the western
world, interest in plants as medications has grown in recent years. In the
global setting, herbal remedies are widely used as the preferred therapeutic
approach worldwide. The increased popularity of natural products among
consumers has led to an increase in demand for herbal medications in recent
years.
Figure 4
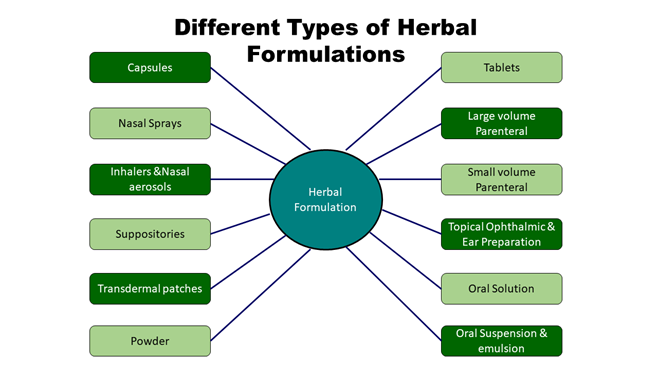
|
Figure 4 Various Types of Herbal Formulations |
On the other hand,
the increasing demand for herbal medicines has led to the systematic
large-scale production in a variety of forms, including pills, capsules,
ointments, nasal sprays, ophthalmic preparations, oral suspensions, powders,
transdermal patches, and more (Figure 4). Among these, herbal products related to
liver have the largest global commercial market Bramhankar et al. (2021). Thus, even in affluent countries, the
public's use of plant-based crude extracts for self-medication is increasing
and is currently being accepted as an alternative to traditional medicine Chaudhary & Kumari (2022).
It is projected
that the global market for herbal drugs will grow significantly between 2024
and 2031. The market is anticipated to expand beyond the estimated horizon in
2022 due to the constant growth rate and increasing adoption of tactics by
major players. Herbal liver medications are currently in high demand and have a
promising future Debnath et al. (2024).
8. Summary and conclusion
Developing nations are facing challenges in various areas like controlling population growth, rising poverty and pollution. The rising cost of medications and their side effects add to the burden which has resulted in popularity of PHFs as these formulations are aligned with the Ayurvedic Principles such as Tridoshas and Panchamahabhutas. Moreover, with advancement in scientific knowledge the phytoconstituents have been identified and formulated in synergistic combination thereby enhancing the efficacy and working as an acceptable alternative. The issue of antibiotic resistance has also led to the exploration of alternative or replacement therapy and PHFs have been able to fill-up the gap. PHFs simultaneously can help in boosting immunity as well as providing antimicrobial, antioxidative, and anti-inflammatory action. Although, PHFs are efficacious and safe but with responsible and well-informed approach they can provide life support and well-being at global level. Public awareness, responsible manufacturing and stringent regulatory control can ensure that formulations meet international standard and can work as adjuvant therapy to mitigate the health problems of mankind.
CONFLICT OF INTERESTS
None.
ACKNOWLEDGMENTS
The authors are thankful to Dr. Atiskumar Chattopadhyay, Former Principal Secretary, Faculty of Science, Jadavpur University, Kolkata-700032 for his guidance and valuable suggestions in carrying out this study. The authors also express their heartfelt thanks to Mr. Gautam Dey, M.D., Mr. Ranajit Dey, Jt. M.D. and Mr. Sumitro Nag, Chief Operating Officer (COO) of Dey’s Medical and management of RCCIIT for facilities and encouragement during this investigation.
REFERENCES
Abbas, S.A., Khan, A., Kalusalingam, A., Menon, B., Siang, T., & Mohammed, J.S. (2023, Jan 16). Pharmacological Screening of Polyherbal Formulation for Hepatoprotective Effect Against Anti Tuberculosis Drugs Induced Hepatotoxicity on Albino Rats. Journal of Survey in Fisheries Sciences, 4313-8.
Abraham, R., & Paridhavi, M. (2013). A Review of Comprehensive Study on Medicinal Plants of Polyherbal Formulation- Churna. Asian J Pharm Clin Res, 6(4), 11-18.
Akbarzadeh, T., Sabourian, R., Saeedi, M., Rezaeizadeh, H., Khanavi, M., & Ardekani, M.R. (2015, Mar 1). Liver Tonics: Review of Plants Used in Iranian Traditional Medicine. Asian Pacific Journal of Tropical Biomedicine, 5(3), 170-81. https://doi.org/10.1016/S2221-1691(15)30002-2
Aladejana, E.B. (2023). Biological Properties of Polyherbal Formulations: A Review of their Antimicrobial, Anti-Inflammatory, Antioxidant, and Toxicological Activities. Pharmacognosy Journal, 15(5). https://doi.org/10.5530/pj.2023.15.178
Ali, M.I., & Kumar, M. (2015). A Recent Update on Hepatoprotective Potential of Herbal Plant. International Journal of Environmental Science and Technology, 1, 25-50.
Ali, S.A., & Datusalia, A.K. (2024, Apr 6). Protective Effects of Tinospora Cordifolia Miers Extract Against Hepatic and Neurobehavioral Deficits in Thioacetamide-Induced Hepatic Encephalopathy in Rats Via Modulating Hyperammonemia and Glial Cell Activation. Journal of Ethnopharmacology, 323. https://doi.org/10.1016/j.jep.2023.117700
Alvari, A., Ahmad, F.J., & Abdin, M.Z. (2012, Aug 1). Contemporary Overview on Clinical Trials and Future Prospects of Hepato-Protective Herbal Medicines. Reviews on Recent Clinical Trials, 7(3), 214-23. https://doi.org/10.2174/157488712802281240
Belapurkar, P., Goyal, P., & Tiwari-Barua, P. (2014). Immunomodulatory Effects of Triphala and Its Individual Constituents: A Review. Indian Journal of Pharmaceutical Sciences, 76(6), 467-475.
Benzie, I.F.F., & Wachtel-Galor, S. (2011). Herbal Medicine: Bimolecular and Clinical Aspects, (2nd Ed). CRC Press/Taylor & Francis. https://doi.org/10.1201/b10787
Bhope, S.G., Nagore, D.H., Kuber, V.V., Gupta, P.K., & Patil, M.J. (2011). Design and Development of a Stable Polyherbal Formulation Based on the Results of Compatibility Studies, Pharmacognosy Res, 3(2), 122-129. https://doi.org/10.4103/0974-8490.81960
Bramhankar, R., Baruah, H., & Munishwar, N. (2021, Apr 1). Insight into Traditional Dosage Forms in light of Ayurvedic Pharmaceutics. International Journal of Pharmaceutical Research, 13(2). https://doi.org/10.31838/ijpr/2021.13.02.499
Chaudhary, R., & Kumari, P. (2022). Stability Aspects of Herbal Formulation. WJPLS, 8(2), 103-10.
Chorgade, M.S. (2007). Drug Discovery and Development: Drug Development Vol. 2. John Wiley and Sons Inc, Hoboken, New Jersey.
Darbar, S. D., Saha, S., Chattopadhyay, S., & Chattapadhyay, A. (2020). Anti-Stress Activity (in-vivo) of Multi Herbal Capsule-Trasina® in Experimental Murine Model. Asian Journal of Pharmaceutical Research and Development, 8(5), 52–58. https://doi.org/10.22270/ajprd.v8i5.839
Darbar, S., & Chattopadhyay, S. (2010). Antiulcer Effect of Livina, A Herbal Formulation Against Ethanol Induced Acute Gastric Ulcer in Mice. Int. J. Pharm, 2(10), 93-100.
Darbar, S., Bhattacharya, A., & Chattopadhyay, S. (2010 Dec). Ameliorative Effect of Livina, a Polyherbal Preparation on Diclofenac-Induced Liver Injury: A Comparison with Silymarin. J Pharm Res, 3(12), 2794-8.
Darbar, S., Bhattacharya, A., Chakraborty, M.R., & Chattopadhyay, S. (2010). Livina, a Polyherbal Preparation Protects Liver Against Aceclofenac-Induced Hepatic Insult in Sprague-Dawley Rats: A Comparison with Silymarin. Pharmacologyonline, 889-907.
Darbar, S., Chakraborty, M.R., Chattarjee, S., & Ghosh, B. (2009). Protective Effect of Livina, A Polyherbal Liquid Formulation Against Ethanol Induced Liver Damage in Rats. Ancient Science of Life, 28(3), 14-17.
Darbar, S., Saha, S., Pramanik, K., & Chattopadhyay A. (2021, Dec). Antioxidant and Immunomodulatory Effect of AKSS16-LIV01-A Multi Herbal Formulation Against Ethanol Induced Liver Dysfunction in Mice. Clinical Phytoscience, 7, 1-20. https://doi.org/10.1186/s40816-021-00312-1
Darbar, S., Saha, S., Pramanik, K., & Chattopadhyay, A. (2000). Preliminary Assessment of Acute and 28-Day Repeated Dose Oral Toxicity of a Newly Developed Herbal Mixture on Experimental Animal. Indian Journal of Pharmaceutical education and Research, 54(1), 135-42. https://doi.org/10.5530/ijper.54.1.16
Darbar, S., Saha, S., Pramanik, K., & Chattopadhyay, A. (2018). Preliminary Acute Oral Toxicity Study of a Newly Developed Herbal Formulation. World J Pharm Res, 7(5), 924-30.
Darbar, S., Saha, S., Pramanik, K., & Chattopadhyay, A. (2020, Nov 15). Ameliorative Efficacy of Novel Multi Herbal Formulation (AKSS16-LIV01) Upon Haematological Modulations Induced by Fixed Dose Combination of Tramadol Hydrochloride/Paracetamol (THP). Journal of Drug Delivery and Therapeutics, 10(6), 11-7. https://doi.org/10.22270/jddt.v10i6.4516
Darbar, S., Saha, S., Pramanik, K., & Chattopadhyay, A. (2021, Jan 1). Ameliorative Effect of Multi Herbal Formulation on Lipid Peroxidation and Redox Dysfunction in Ethanol Induced Hepatic Imbalance. Indian Journal of Pharmaceutical Education and Research, 55(1), 215-23. https://doi.org/10.5530/ijper.55.1.24
Debnath, B., Manna, K., Singh, W.S., & Goswami, S. (2024, Jan 1). Formulation and Evaluation of New Herbal Nutraceutical Tablet for the Treatment of Diabetes Mellitus. Journal of Drug Research in Ayurvedic Sciences, 9(1), 29-39. https://doi.org/10.4103/jdras.jdras_48_23
Farnsworth, N.R., Akerele, O., Bingle, A.S., Sojarto, D.D., & Guo, Z. (1985). Medicinal Plant in Therapy. Bulletin of the World Health Organization, 63, 965-981.
Gaurav, Sharma, I., Khan, M.U., Zahiruddin, S., Basist, P., & Ahmad, S. (2023, Jan 9). Multi-Mechanistic and Therapeutic Exploration of Nephroprotective Effect of Traditional Ayurvedic Polyherbal Formulation using in Silico, in Vitro and in Vivo Approaches. Biomedicines, 11(1), 168. https://doi.org/10.3390/biomedicines11010168
Ghosh, N., Ghosh, R., Mandal, V., & Mandal, S.C. (2011). Recent Advances in Herbal Medicine for Treatment of Liver Diseases. Pharmaceutical Biology, 49(9), 970-988. https://doi.org/10.3109/13880209.2011.558515
Girish, C., & Pradhan, S.C. (2017, Jan 1). Herbal Drugs on the Liver. InLiver pathophysiology. Academic Press, 605-620. https://doi.org/10.1016/B978-0-12-804274-8.00044-8
Hamid, K.M., Shehu, A.A., Kalgo, M.U., Isiyaku, A., Alkali, S., Muhammad, T., Usman, A. B.,Isah, S. Y., & Abubakar, N. K. (2021). Immunomodulatory Activity of Aqueous Extract of Polyherbal Formulation on Macrophage Function and Humoral Immune Response Against SRBCs in Mice. Nigerian Journal of Pure and Applied Sciences, 34(2), 3989-3997. https://doi.org/10.48198/NJPAS/21.A01
Ingawale, D.K., Shah, P. V., & Patel, S.S. (2015). Hepatoprotective Effect of Virgoliv Syrup Against CCL4 Induced Hepatic Injury in Rats. International Journal of Pharmacy and Pharmaceutical Sciences, 7(8), 221-226.
Iroanya, O.O., Adebesin, O.A., & Okpuzor, J. (2014). Evaluation of the Hepato and Nephron-Protective Effect of a Polyherbal Mixture using Wistar Albino Rats. Journal of Clinical and Diagnostic Research 8(6), 15-21. https://doi.org/10.7860/JCDR/2014/5875.4501
Kantharia, C., Kumar, M., Jain, M.K., Sharma, L., Jain, L., & Desai, A. (2023, Jul 31). Hepatoprotective Effects of Liv. 52 in Chronic Liver Disease Preclinical, Clinical, and Safety Evidence: A Review. Gastroenterology Insights, 14(3), 293-308. https://doi.org/10.3390/gastroent14030021
Karole, S., Shrivastava, S., Thomas, S., Soni, B., Khan, S., Dubey, J., Dubey, S.P., Khan, N., & Jain, D.K. (2019 Feb). Polyherbal Formulation Concept for Synergic Action: A Review. Journal of Drug Delivery and Therapeutics, 15(9)(1-s), 453-66. https://doi.org/10.22270/jddt.v9i1-s.2339
Khan, M.U., Basist, P., Zahiruddin, S., Penumallu, N.R., & Ahmad, S. (2024, Jan 10). Ameliorative Effect of Traditional Polyherbal Formulation on TNF-α, IL-1β and Caspase-3 Expression in Kidneys of Wistar Rats Against Sodium Fluoride Induced Oxidative Stress. Journal of Ethnopharmacology, 318. https://doi.org/10.1016/j.jep.2023.116900
Kotmire, S., Desai, A., & Chougule, N. (2024). The Advances in Polyherbal Formulation. Journal of Pharmacognosy and Phytochemistry, 13(1), 210-21. https://doi.org/10.22271/phyto.2024.v13.i1c.14828
Kunwar, R.M., Shrestha, K.P., & Bussmann, R.W. (2010). Traditional Herbal Medicine in Far-West Nepal: A Pharmacological Appraisal. J Ethnobiol Ethnomed, 6, 35. https://doi.org/10.1186/1746-4269-6-35
Lakshmi, P.V., Krishnan, S.A., & Srilakshmi, S. (2023, Nov 16). Hepatoprotective Activity of Polyherbal Formulation Encompassing Original Therapeutic Plants in Rats. Journal of Research Administration, 5(2), 1415-21.
Ngo, L.T., Okogun, J.I., & Folk, W.R. (2014). 21st Century Natural Product Research and Drug Development and Traditional Medicines. Nat Prod Rep, 30(4), 584-92. https://doi.org/10.1039/c3np20120a
Padmanabhan, P. & Jangle, S.N. (2014). Hepatoprotective Activity of Herbal Preparation (HP-4) Against Carbontetrachloride Induced Hepatotoxicity in Mice. Journal of Chemical and Pharmaceutical Research, 6(2), 336-346. https://doi.org/10.3126/ijasbt.v2i1.9346
Parasuraman, S., Thing, G.S., & Dhanaraj, S.A. (2014). Polyherbal Formulation: Concept of Ayurveda Pharmacogn Rev, 8(16), 73-80. https://doi.org/10.4103/0973-7847.134229
Parveen, A., Singh, A., Rajendiran, A., Jough, S.S., & Verma, S.K. (2022). Herbal Elicited Hepatoprotection and Hepatotoxicity-A Comprehensive Review. Asian Journal of Pharmaceutical Research, 12(2), 155-61. https://doi.org/10.52711/2231-5691.2022.00024
Pingale, S.S., Pokharkar, R.D., & Pingale, M.S. (2008). Standardisation of Herbal Drug as a Potent Liver Tonic. Pharmacologyonline Newsletter, 1, 13-9.
Rajanna, M., Bharathi, B., Shivakumar, B.R., Deepak, M., Prashanth, D.S., Prabakaran, D., Vijayabhaskar, T., Arun, B. (2021). Immunomodulatory Effects of Andrographis Paniculata Extract in Healthy Adults - An Open-Label Study. Journal of Ayurveda and Integrative Medicine, 12(3), 529-534. https://doi.org/10.1016/j.jaim.2021.06.004
Ramaiah, M., Chakravathi, G., & Yasaswini, K. (2013). In Vitro Biological Standardization, Formulation and Evaluation of Directly Compressed Polyherbal Anthelmintic Tablets. Pharmacogn J, 5(3), 130-4. https://doi.org/10.1016/j.phcgj.2013.04.004
Rastogi, S., Chiappelli, F., Ramchandani, M.H., & Singh, R.H. (2012). Evidence-Based Practice in Complimentary and Alternative Medicine Perspective, Protocols, Problems and Potential in Ayurveda. New York City: Springer.
Saha, S. & Ghosh, S. (2012). Tinospora Cordifolia: One Plant, Many Roles. Ancient Science of Life 31(4), 151. https://doi.org/10.4103/0257-7941.107344
Saleem, U., Usman, M., Anwar, F., Akhtar, M.F., & Ahmad, B. (2020). Pharmacological and Toxicological Evaluation of Two Anti-Asthmatic Polyherbal Formulations. Anaisda Academia Brasileira de Ciencias, 92(3), 1-13. https://doi.org/10.1590/0001-3765202020191562
Sane, R.T. (2002). Standardization, Quality Control and GMP for Herbal Drug. Indian Drugs, 39(3), 184-190.
Sarwar, M., Attitalla, I.H., & Abdollahi, M. (2011). A Review on the Recent Advances in Pharmacological Studies on Medicinal Plants: Animal Studies are Done but Clinical Studies Needs Completing. Asian J Anim Vet Adv, 6(8), 867-883. https://doi.org/10.3923/ajava.2011.867.883
Shaik, A.A., Elumalai, A.A., Eswaraiah, M.C., & Swathi, S. (2012). An Updated Review on Hepatoprotective Medicinal Plants. Journal of Drug Delivery and Therapeutics, 13, 2(2). https://doi.org/10.22270/jddt.v2i2.97
Shakya, A.K., Sharma, N., Bhadauria, M., Nirala, S.K., Shrivastava, S., & Shukla, S. (2022, Oct). Ameliorative Impact of Herbal Formulation-Majoon-Dabeed-Ul-Ward and Sharbat-e-Deenar Against CCl4 Induced Liver Toxicity Via Regulation of Antioxidant Enzymes and Oxidative Stress. Toxicology Research, 11(5), 819-30. https://doi.org/10.1093/toxres/tfac052
Sharma, A.K., Kaur, S., Kohli, N., Sharma, I., Sharma, S. & Verma, S.K. (2015). Evaluation of Hepatoprotective Efficacy of Polyherbal Formulation "Amlycure DS" on Anti- Tubercular Drug (ATT) Induced Hepatotoxicity. Asian Journal of Biochemical and Pharmaceutical Research, 5(3), 238-254.
Siddiqui, S., Rahman, M., Islam, S., Islam, S., Hasan, M.M., & Rahman, M.M. (2017). Biological Effects of Commercial Enzymes, Probiotics and Liver Tonic on Live Weight and Hematobiochemical Parameters in Broiler. Int J Res Agri Sci, 4(1), 56-9.
Singh, D., Khan, M.A., & Siddique, H.R. (2024, Jan). Unveiling the Therapeutic Promise of Natural Products in Alleviating Drug-Induced Liver Injury: Present Advancements and Future Prospects. Phytotherapy Research, 38(1), 22-41. https://doi.org/10.1002/ptr.8022
Singh, N., Gupta, P., Bharti, C., & Shanmugam, S.K. (2023, Jul 1). Evaluation of Hepatoprotective Efficacy of a Polyherbal Unani formulation Majoon-Najah Against Cadmium Chloride-Induced Liver Damage. Current Drug Research Reviews Formerly: Current Drug Abuse Reviews, 15(2), 188-98. https://doi.org/10.2174/2589977515666221207141645
Sivakumar, V., Rajan, M.D., Sadiq, A.M. & Rajeshkumar, S. (2014). Hepatoprotective Effect of Polyherbal Formulations in Paracetamol Induced Hepatic Damaged Experimental Rats. International Research Journal of Pharmaceutical and Biosciences, 1(1), 30-35.
Spinella, M. (2002). The Importance of Pharmacological Synergy in Psychoactive Herbal Medicines. Altern Med Rev, 7, 130-137.
Stickel, F., & Schuppan, D. (2007). Herbal Medicine in the Treatment of Liver Diseases. Digestive and Liver Disease, 39(4), 293-304. https://doi.org/10.1016/j.dld.2006.11.004
Vargas-Pozada, E.E., & Muriel, P. (2020, Feb). Herbal Medicines for the Liver: From Bench to Bedside. European Journal of Gastroenterology & Hepatology, 1, 32(2), 148-58. https://doi.org/10.1097/MEG.0000000000001485
Yadav, R., Yadav, N., & Kharya, M.D. (2016). Immunomodulation Potential of Andrographis Paniculata and Tinospora Cordifolia Methanolic Extracts in Combination Forms. International Journal of Pharmacological Research 6(09), 121-125.
 This work is licensed under a: Creative Commons Attribution 4.0 International License
This work is licensed under a: Creative Commons Attribution 4.0 International License
© Granthaalayah 2014-2024. All Rights Reserved.